Further Reading
- What to Expect After Cataract Surgery
- Medicaid Coverage
- Cataract Surgery After Vitrectomy
- Age Limit
- Headache After Surgery
- Surgery & Blood Thinners
- Common & Uncommon Complications
- Lens Options for Babies with Congenital Cataracts
- Cataract Evaluation: What to Expect & Why You Should Get Tested
- What to Expect with Cataract Surgery: Before, During and After the Procedure
- Alternatives to Surgery
- Cataract Surgery Risks
- Comparing Surgical Methods
- Laser Vs. Traditional Surgery
- Steps to the Surgery
- Laser Surgery for Cataracts
- Multifocal IOLs
- Extended Depth of Focus IOLs
- How Long to Wait Before Exercise
- Superficial Keratectomy Before Cataract Surgery
- What to Expect From Cataract Surgery Anesthesia
- Cataract Surgery and Floaters
- Cataract Surgery Cost: Insurance Coverage and Out of Pocket Expenses
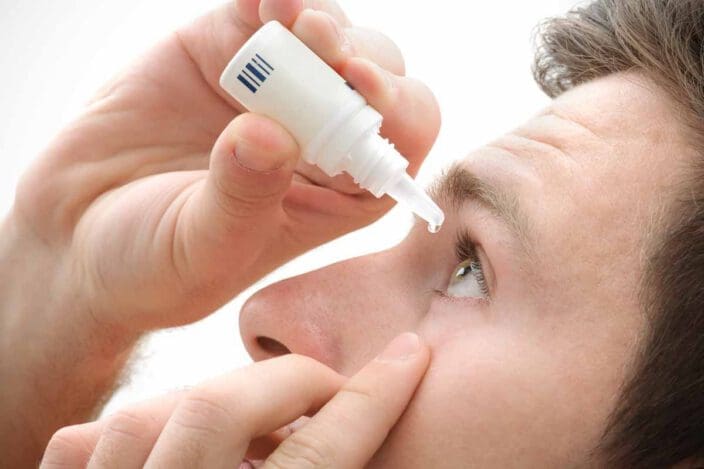
Best Eye Drops After Cataract Surgery
Home / Guide to Cataract Surgery /
Eye drops are critical after cataract surgery. Antibiotic drops prevent infection. Steroid drops ease inflammation. And both keep tissues lubricated and hydrated.
If your eyes still feel sticky and sore despite your drops, talk to your doctor. Don’t buy or use over-the-counter lubricating drops without checking first. Some products have been recalled due to contamination concerns.
Table of Contents
What Are the Best Eye Drops to Use After Cataract Surgery?
The best eye drops after cataract surgery are those your doctor prescribes. Typically, your doctor will recommend one drop to prevent infection and another to reduce inflammation.
Every year, about 1 million cataract surgeries are performed. The procedure is safe, effective, and the only way to address eyes clouded by cataracts. But your aftercare is critical for the best results.
During cataract surgery, your doctor will make a small incision and remove the clouded lens. An artificial intraocular lens (IOL) replaces it. You’re sent home the same day to heal and rest. Your doctor will provide eye drops and a schedule for their use.
Antibiotic Eye Drops
During cataract surgery, your doctor makes a tiny incision in your eye. That cut can allow bacteria to enter your eye.
Infections are serious complications. Thankfully, they’re very rare, occurring in less than 1% of patients. Antibiotic eye drops can help keep you safe.
NVISION doctors use two types of antibiotic medications. One is a combination therapy, and the other is a standalone antibiotic. Your doctor will choose which version is right for you.
| Medication | Medication Type | Average Price | Side Effects |
| Ofloxacin (Floxin and Ocuflox) | Antibiotic | $12 | Stinging, blurry vision, watery eyes, light sensitivity |
| Pred-Moxi (prednisolone acetate and moxifloxacin) | Antibiotic/steroid combination | $25 | Blurry vision, dry eyes, broken blood vessels in the eyes, eye tenderness |
Steroid Eye Drops
Your body reacts to injuries with swelling. Puffy tissues immobilize wounds and speed healing. But too much inflammation can harm your recovery and cause more problems. Steroid eye drops ensure your eyes don’t swell too much.
Steroid eye drops can also reduce pain after surgery. Using them can keep you comfortable as you heal.
NVISION doctors use two medications in this class. One is a combination product that contains an antibiotic too. The other is a standalone steroid. Your doctor will help you decide which is best for you.
| Medication | Medication Type | Average Price | Side Effects |
| Prednisolone | Steroid | $12 | Itchy eyes, change in vision, difficulty focusing, drooping of the eyelids |
| Pred-Moxi (prednisolone acetate and moxifloxacin) | Antibiotic/steroid combination | $25 | Blurry vision, dry eyes, broken blood vessels in the eyes, eye tenderness |
How to Apply Eye Drops After Surgery

Post-cataract surgery care is important. Your doctor will provide detailed instructions to follow after surgery. Ensure you understand those recommendations before you go home so you know what to do.
To use your eye drops, follow these steps:
- Wash your hands thoroughly. You will be touching parts of your eyes in the process.
- Sit down and tilt your head back, or lie down instead.
- Pull your lower eyelid down gently.
- Use your nose or forehead to brace your hand and keep it steady.
- Squeeze a drop into your eye, taking care not to touch the surface with the bottle’s tip.
- Close your eyes for a moment. Blink, and then close your eyes again.
- Blot excess drops with tissues.
- Wait a few minutes before applying drops of a second type (if applicable).
Keep track of when you use each drop by writing down the time or marking the dose on your phone. If you’re worried you might forget your doses, set timers with your phone to stay on track.
Most people use eye drops for several weeks after surgery. Don’t stop using them until your doctor tells you it’s safe to do so.
Should You Use Lubricating Eye Drops After Cataract Surgery?

Itchiness and dryness are common symptoms after eye surgery. Before you reach for over-the-counter lubricating drops, ask your doctor.
In early 2023, several eye drop products sold in the United States were recalled due to associated illness. Some people who used these drops developed severe infections that put their vision at risk.
Complications with cataract surgery are very rare. But putting a contaminated product into an eye healing from surgery could lead to serious problems. To stay safe, ask your doctor before putting anything in your eyes.
Eye Drops After Cataract Surgery Frequently Asked Questions
Yes. Eye drops can help keep you comfortable as tissues heal. Some can reduce the risk of infection too.
Your risk of complications, including infections and poor tissue healing, can rise if you don’t follow your doctor’s instructions. This can also be very painful.
Yes. Your doctor might apply your first dose before you go home after surgery. But you’ll start using the products when you get home.
Most people use eye drops for several weeks after cataract surgery. Your doctor will create a plan just for you and your eyes.
References
- Future of Cataract Surgery Seems Promising. (February 2021). Healio.
- Postoperative Endophthalmitis After Cataract Surgery: An Update. (February 2022). Cureus.
- What to Know About the 2023 Eye Drop Recalls, Understanding the Risks. (April 2023). Pharma News Intelligence.
The information provided on this page should not be used in place of information provided by a doctor or specialist. To learn more, read our Privacy Policy and Editorial Policy pages.
Further Reading
- What to Expect After Cataract Surgery
- Medicaid Coverage
- Cataract Surgery After Vitrectomy
- Age Limit
- Headache After Surgery
- Surgery & Blood Thinners
- Common & Uncommon Complications
- Lens Options for Babies with Congenital Cataracts
- Cataract Evaluation: What to Expect & Why You Should Get Tested
- What to Expect with Cataract Surgery: Before, During and After the Procedure
- Alternatives to Surgery
- Cataract Surgery Risks
- Comparing Surgical Methods
- Laser Vs. Traditional Surgery
- Steps to the Surgery
- Laser Surgery for Cataracts
- Multifocal IOLs
- Extended Depth of Focus IOLs
- How Long to Wait Before Exercise
- Superficial Keratectomy Before Cataract Surgery
- What to Expect From Cataract Surgery Anesthesia
- Cataract Surgery and Floaters
- Cataract Surgery Cost: Insurance Coverage and Out of Pocket Expenses