Medically Reviewed by Tom Tooma, M.D., Founder/Medical Director NVISION Surgeon
Does Coronavirus Affect Your Eyes or Vision?
Home /
Last Updated:
Medically Reviewed by Tom Tooma, M.D., Founder/Medical Director NVISION Surgeon
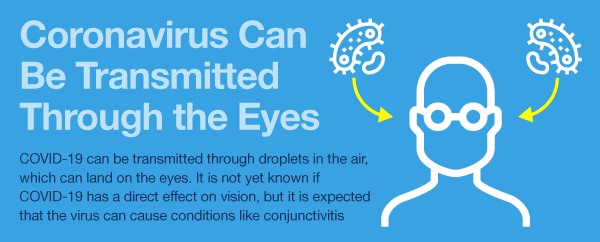
COVID-19 can be transmitted through droplets in the air, which can land on the eyes. While it is rare to contract COVID-19 through the eyes, it is possible.
In rare cases, the virus can cause conditions like conjunctivitis. Symptoms of conjunctivitis include pain and temporary loss of vision. Some people have reported lingering eye issues after COVID-19 infection, such as light sensitivity, limited depth perception, and pain.
Table of Contents
The State of Coronavirus
At this point in the pandemic, people are familiar with the most common symptoms of COVID-19, such as fever, loss of sense of smell and taste, and fatigue. COVID-19 can cause mild respiratory problems in some humans while leading to more serious and life-threatening conditions (such as pneumonia, bronchitis, and kidney failure) in others.
As of August 2021, 70 percent of adults in the US have received at least one dose of the coronavirus vaccine. While the delta variant is causing the number of cases in the US to surge, vaccination still proves to be the best way to prevent the spread of the virus.
You deserve clear vision. We can help.
With 135+ locations and over 2.5 million procedures performed, our board-certified eye surgeons deliver results you can trust.
Your journey to better vision starts here.
According to the World Health Organization, the basic symptoms of COVID-19 mimic those of the flu. People will usually be fatigued, experience a cough, and run a temperature. Some people might feel pain in their bones and joints. Some might have diarrhea. Symptoms usually start out quite mild and then gradually build up.
There is a subset of the population that will become infected by COVID-19 but won’t develop any symptoms or experience any malaise. However, they might still unknowingly pass on COVID-19 to other people, including those in poor health or with weakened immune systems.
As many as 80 percent of the people who get COVID-19 will recover without significant treatment. People over the age of 60 and people with underlying medical conditions may develop a serious illness or have their pre-existing condition exacerbated by COVID-19.
Does Coronavirus Affect the Eyes or Vision?

While there haven’t been widespread reports of vision and eye issues related to COVID-19, ophthalmologists are very concerned about how the disease might affect the eyes and vision. man rubbing eyesA new study shows that people who suffer from severe COVID-19 infections may be at heightened risk for certain eye abnormalities, such as nodules at the back of the eye. Researchers think the nodules may be linked to inflammation related to COVID-19 as well as poor vein drainage around the eyes due to being in a prone position for long periods of time.
It’s recommended that patients with severe COVID-19 have regular eye exams to monitor any ocular developments.
There have been anecdotal reports of patients who have experienced lingering effects on vision from COVID-19, such as light sensitivity, pain, migraines, and difficulties with depth perception. These symptoms are common in people who experience a traumatic brain injury (TBI). Light therapy treatments may help, but researchers are still observing this effect of COVID-19 and potential therapies.
In March 2020, researchers writing in the Ocular Immunology and Inflammation journal said that, to their understanding, “there have been anecdotal reports of ocular infection” stemming from transmission of COVID-19. The researchers writing the article suggested that the longer COVID-19 goes without treatment, the more likely it is that patients will develop infection of the eye tissue as a result of the virus.
Conjunctivitis & Coronavirus
One such condition is conjunctivitis, which is inflammation of the conjunctiva (the thin sheet of tissue) of the eyeball. Conjunctivitis is normally caused by irritants, bacteria, and viruses, so COVID-19 might be a factor in its development.
The infection can make the eye look infected and red, so it is informally known as pink eye. Patients experience a burning sensation in the affected eye, often making it painful to keep the eye open.
The virus also inflames the tiny oil glands near the base of the eyelashes, causing a liquid discharge that can harden into a crust (a condition known as blepharitis). For this reason, many patients with conjunctivitis will wake up to their eyelashes being “crusted over,” trapping the eyelids closed. The crust can be broken up and washed away with warm water.
Conjunctivitis caused by a viral infection can lead to upper respiratory infections in patients, triggering colds and flu-like symptoms. This might be a sign of the presence of COVID-19.
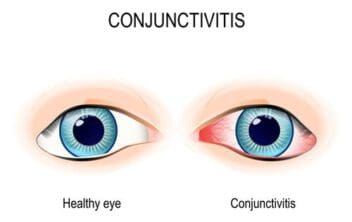
A 2020 study published in the New England Journal of Medicine on the “clinical characteristics of coronavirus disease” across hospitals in China found the typical red, infected eyes of conjunctivitis (or more specifically, “conjunctival congestion”) in 0.8 percent of patients with confirmed COVID-19 infections.
Transmission Through the Eyes
Similarly, the Journal of Medical Virology published a report that concluded that the SARS-CoV-2 coronavirus might possibly be detected in the conjunctival secretions (tears) of patients who have novel coronavirus pneumonia. Researchers found that COVID-19 was not detected in patients who had novel coronavirus pneumonia but did not have conjunctivitis. Even though this study of 30 patients hospitalized for COVID-19 found only one patient diagnosed with conjunctivitis, the researchers were still concerned that “the possibility of eye infection” was significant enough to warrant protection when treating patients.
The concern is based on the story of a respiratory specialist named Wang Guangfa, who was not wearing any kind of protective eyewear when he came into contact with COVID-19 patients in China. Wang’s left eye became inflamed after his exposure to the patients. He developed a fever and an accumulation of mucus in his nose and throat, subsequently becoming a confirmed COVID-19 case himself.
Ophthalmologists writing in The Lancet concluded that “unprotected exposure of the eyes to [COVID-19] … might have allowed the virus to infect the body.” They further declared that, as eye specialists, it was their professional belief that “transmission of [COVID-19] through the eyes was ignored.”
You deserve clear vision. We can help.
With 135+ locations and over 2.5 million procedures performed, our board-certified eye surgeons deliver results you can trust.
Your journey to better vision starts here.
Protecting the Eyes From COVID-19
Doctors are encouraging COVID-19 patients and other vulnerable people to protect their eyes during the outbreak, and this is particularly true during the recent surge from the delta variant. Virus particles can be sprayed through the act of sneezing, coughing, or even talking into another person’s face.

Usually, the droplets are unwittingly inhaled through the mouth or nose, but they can also affect the eyes, possibly causing conjunctivitis (among other eye conditions) and also transmitting the disease itself. The infection can also be passed by touching a surface that has the virus on it (like a doorknob or smartphone screen) and then touching the eyes.
If a person tests positive for COVID-19, they should not visit their optometrist in person until the infection clears. As the Ophthalmology Times writes, “ophthalmologists can be at risk each time they see a patient who may be exhibiting symptoms of the disease.”
How to Get Help for Your Eyes
Despite the new guidelines for patient treatment during the pandemic, if a patient is experiencing pain in their eyes or loss of vision, they should call their ophthalmologist for guidance. Changes in vision or macular degeneration (an eye disease that develops in people over age 60, who are also at increased risk for contracting COVID-19) are also good reasons to call a doctor or ophthalmologist.
Even if your doctor encourages you to come in for an examination, the intake process will likely be very different as a way of reducing the transmission of the SARS-CoV-2 virus. For example, your clinic may ask you to wait in your car to limit the number of people who are inside the facility at any given time. Doctors will be equipped with a plastic breath shield while they examine your eyes, and they may wear their own eye protection as well.
You might even be asked not to speak during the exam, to reduce the risk of exposing your doctor to any droplets containing the COVID-19 virus, if that is what you have that is causing disruptions to your vision or distress to your eyes. The conversation itself might take place under social distancing guidelines, where you and your doctor will sit six feet apart from each other.

If possible, your doctor’s practice might conduct the examination via telemedicine, over a consumer-based or telehealth video conferencing app. This will allow for you to get “looked at” even if you have to self-quarantine. Specific offices have different policies on this, and guidelines have changed often throughout the pandemic, depending on current rates. Contact your ophthalmologist or optometrist to learn how they are handling office visits during the pandemic.
Eye Care During the COVID-19 Outbreak
The American Academy of Ophthalmology suggests that people can help their eye health, and the eye health of others, by following some simple steps during the COVID-19 outbreak.
- Choose eyeglasses. If you wear contact lenses, use your glasses instead. This will reduce the number of times you have to touch your eyes, helping to reduce the risk of infection. While there is no evidence to suggest that wearing contacts increases your risk of contracting COVID-19, glasses may partially protect your face from respiratory droplets.
- Stock up on critical eye medicine prescriptions. Supplies can be limited during the quarantine, and if you have to self-isolate, you will not be able to pick up a prescription. Patients with insurance that allows them to get more than a month’s supply of vital eye medicine should get as much as they can. Some insurance companies will allow patients to get up to three months’ worth of medication in an emergency. Patients should also request a refill as soon as their supplies run low.
- Wash your hands. Regular hand washing (for at least 20 seconds at a time) is incredibly important. If you don’t have access to soap and water, use hand sanitizer that is at least 60 percent alcohol.
- Avoid touching or rubbing your eyes. This is especially important if you are already sick or you have been near someone who has been coughing or sneezing. This can be very difficult since studies show the average person touches their face 23 times per hour. If you must touch your eyes, use a tissue instead of your fingers. Then, dispose of the tissue. If you need to administer eye medicine or eye drops, you should first wash your hands with soap and hot water for 20 seconds. Then, wash your hands again after administering the medication.
- Take additional precautions. Stay six feet away from other people; avoid large crowds; and sneeze into your elbow or a tissue. Regularly clean your house and disinfect frequently used surfaces. Steer clear of people who might be sick.
All these measures will reduce the possibility of transmitting COVID-19 and help to protect your eyes and vision during this outbreak.
You deserve clear vision. We can help.
With 135+ locations and over 2.5 million procedures performed, our board-certified eye surgeons deliver results you can trust.
Your journey to better vision starts here.
References
- About the Coronaviridae Family. (March 2020). Virus Pathogen Resource.
- U.S. Hits Biden’s Vaccination Goal a Month Late, With 70 Percent of Adults Receiving at Least One Shot. (August 2021). The Washington Post.
- Q&A on Coronaviruses (COVID-19). (March 2020). World Health Organization.
- Ocular MRI Findings in Patients with Severe COVID-19: A Retrospective Multicenter Observational Study. (February 2021). Radiology.
- One Year After COVID-19 and Fighting for My Vision. American Optometric Association.
- Can the Coronavirus Disease 2019 (COVID-19) Affect the Eyes? A Review of Coronaviruses and Ocular Implications in Humans and Animals. (March 2020). Ocular Immunology and Inflammation.
- What Is Blepharitis? (April 2019). American Academy of Ophthalmology.
- Clinical Characteristics of Coronavirus Disease 2019 in China. (March 2020). New England Journal of Medicine.
- Evaluation Of Coronavirus in Tears and Conjunctival Secretions of Patients With SARS‐CoV‐2 Infection. (February 2020). Journal of Medical Virology.
- 2019-nCoV Transmission Through the Ocular Surface Must Not Be Ignored. (February 2020). The Lancet.
- You Could Be Spreading The Coronavirus Without Realising You’ve Got It. (March 2020). New Scientist.
- Ophthalmologists at Ground Level of COVID-19 Fight. (March 2020). Ophthalmology Times.
- Why Is It So Hard to Stop Touching My Face? (March 2020). USA Today.
- Face Touching: A Frequent Habit That Has Implications for Hand Hygiene. (February 2015). American Journal of Infection Control.
- Coronavirus Could Accelerate Moves Toward “Telemedicine.” (March 2020). Los Angeles Times.
- Coronavirus And Eyes: Experts Recommend Wearing Glasses Instead of Contacts to Prevent COVID-19 Spread. (March 2020). 6 ABC Action News.
- Ask the Expert: How COVID-19 Affects the Eyes. USC Rocki Eye Institute, Keck Medicine of USC.
- Coronavirus: Can It Affect Eyesight? (May 2020). BBC.
- Coronavirus and Your Eyes. American Academy of Ophthalmology.
- Research Reveals How COVID-19 Affects the Eyes. (December 2020). ScienceDaily.
- LA County to Begin Offering 3rd Doses of COVID-19 Vaccine to People With Severe Immune Issues. (August 2021). Los Angeles Daily News.
Dr. Tooma, the founder of NVISION® Eye Centers, has performed well over 130,000 LASIK surgeries, making him the most experienced LASIK surgeon in the Western United States.
This content is for informational purposes only. It may have been reviewed by a licensed physician, but is not intended to serve as a substitute for professional medical advice. Always consult your healthcare provider with any health concerns. For more, read our Privacy Policy and Editorial Policy.

