Medically Reviewed by Salwa Aziz, M.D., M.P.H. NVISION Surgeon
Glaucoma Diagnosis: What You Should Know
Home /
Last Updated:

Medically Reviewed by Salwa Aziz, M.D., M.P.H. NVISION Surgeon

Article At a Glance
Glaucoma is a group of eye conditions that can cause vision loss by damaging the optic nerve—often without early symptoms. This article explains the types of glaucoma, risk factors, and why regular eye exams are crucial for early detection. It also covers treatment options like eye drops, laser procedures, and surgery to manage eye pressure and protect vision. If you have a family history of glaucoma or are over 60, getting checked regularly is key. Early diagnosis and proper treatment can help you preserve your sight and quality of life.
Table of Contents
As of 2022, nearly 4.2 million Americans struggled with glaucoma. That number is expected to rise to over 6 million by 2050, per the National Eye Institute (NEI). Regular eye exams can detect glaucoma. The sooner you are diagnosed and start treatment protocols, the better. While there is no cure for glaucoma, you can greatly slow the progression of the disease.
What Is Glaucoma?
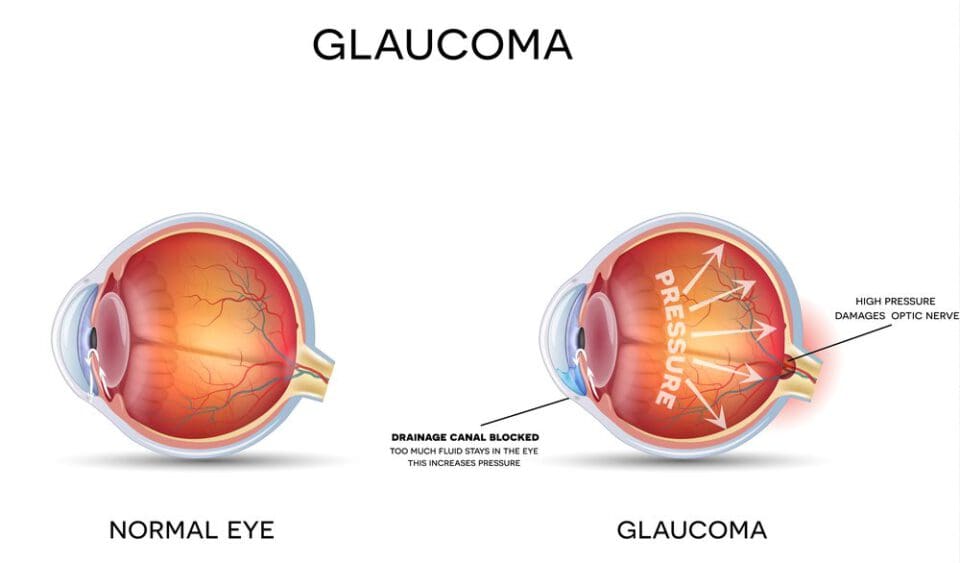
Glaucoma is an eye disease that increases the pressure inside the eye. Over time, increased pressure can cause damage to the optic nerve, leading to blindness.
Your optic nerve sends information from your eyes to your brain to process what you are seeing. A fluid called aqueous humor sits between your cornea and lens inside your eye. If this fluid level gets too high and can’t drain properly, it results in high intraocular pressure (also called IOP). High pressure levels in the eyes can damage the optic nerve or restrict blood flow.
You deserve clear vision. We can help.
With 135+ locations and over 2.5 million procedures performed, our board-certified eye surgeons deliver results you can trust.
Your journey to better vision starts here.
Glaucoma is most common in older adults. In fact, glaucoma is one of the top causes of blindness for those over age 60. Unfortunately, the eye damage and vision loss caused by glaucoma are not reversible, but as soon as it is diagnosed, you can take steps to prevent further damage and at least slow vision loss. Glaucoma is often referred to as the “silent thief of sight” because it can progress without noticeable symptoms in the early stages.
Types of Glaucoma
There are two main types of glaucoma: primary open-angle glaucoma (the most common) and angle-closure glaucoma.
Primary Open-Angle Glaucoma
With primary open-angle glaucoma, there are often no early symptoms. It is caused by the aqueous humor draining too slowly, which is commonly related to a blockage in your drainage angle.
You may lose side and peripheral vision before you even realize that you are suffering from the condition. It can lead to vision loss and blindness without treatment.
Angle-Closure Glaucoma (“Narrow-Angle” Glaucoma)
If your iris is too close to your drainage angle in your eye, it can lead to a buildup of fluid and this form of glaucoma. If you have chronic angle-closure glaucoma, you may not notice any symptoms unless there is an acute attack.
Narrow-Angle Glaucoma is considered an eye emergency, and requires immediate medical care.
Other Types of Glaucoma
Normal Tension Glaucoma
Low blood pressure or limited blood flow can be a risk factor for this type of glaucoma. Normal tension glaucoma is indicated by optic nerve damage without high IOP.
Pigmentary Glaucoma
This type of glaucoma occurs when pigment granules build up in the drainage channels of your eyes, which can slow or block drainage of fluid.
Congenital Glaucoma
An underlying medical condition, defect in the drainage angle, or drainage blockage can damage the optic nerve in children or infants, leading to this form of glaucoma. Typically watery eyes, cloudy corneas, and light sensitivity are indicators of congenital glaucoma.
Secondary Glaucoma
This form of glaucoma is caused by something else, such as an injury to the eye, medical condition, medications, or other eye conditions that can lead to high IOP and damage to the optic nerve.
Risk Factors for Glaucoma
Glaucoma can impact anyone, but there are certain things that can increase the odds for glaucoma. Risk factors include:
- A family history of glaucoma
- Being over age 60
- Being Hispanic or African American and over age 40
- Chronic eye inflammation
- Thinner corneas
- Medication that increases eye pressure
- Medical conditions, such as heart disease or diabetes
- Prolonged use of corticosteroids
- Injury to the eye
- Eye tumors
- Optic nerve sensitivity
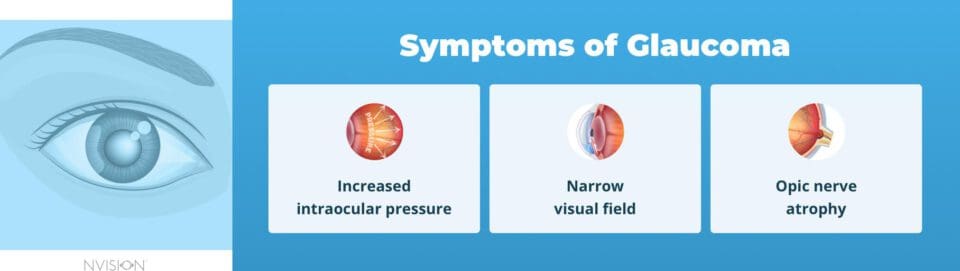
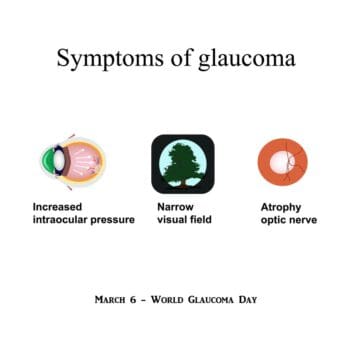
Glaucoma Symptoms
The symptoms of glaucoma can vary depending on the type of glaucoma you have, but there are some key signs to look for:
Symptoms of Open-Angle Glaucoma
- Gradual loss of peripheral vision. Often unnoticeable in early stages as vision loss begins at the edges.
- Tunnel vision in advanced stages. Vision loss can progress until only central vision remains, resembling a “tunnel.”
Symptoms of Angle-Closure Glaucoma
- Severe eye pain. Sudden, intense eye pain due to rapid eye pressure increase.
- Headache accompanying eye pain. Pain often spreads to the head, worsening with the eye discomfort.
- Nausea and vomiting from severe pain. Discomfort can lead to feelings of nausea and vomiting.
- Blurred vision with sudden onset. Vision becomes cloudy or unclear, often very rapidly.
- Halos or rainbow rings around lights. Lights appear surrounded by halos or rainbow-like rings.
- Redness in the eye. The eye may appear visibly red due to increased pressure.
Causes of Glaucoma
Glaucoma occurs when your optic nerve is damaged. Millions of nerve fibers make up your optic nerve, and high intraocular pressure can cause them to die off. This can create blind spots in your vision. If the increased pressure continues unchecked, it can result in blindness.
The fluid in your eye, called aqueous humor, is constantly being produced. It flows into the eye and should drain out at equal rates. If the drainage angle becomes blocked, it can lead to fluid buildup, which raises your IOP and damages your optic nerve.
Glaucoma can run in families, so there is a potential genetic link. It can also be caused by medical conditions, trauma to the eye, or medications.
Diagnosing Glaucoma
Unfortunately, there are often no early warning signs or symptoms of glaucoma. The best thing you can do to manage it is to catch it as early as possible, so regular eye exams are essential. Your optometrist or ophthalmologist will use an instrument called a tonopen that measures your IOP, typically after using eye drops to dilate your pupils.
If your pressure is high – above 21 mmHg (millimeters of mercury) – it can be a sign of glaucoma. Imaging technology and peripheral vision field tests can also be used to diagnose glaucoma.
About half of the people living with glaucoma do not even realize it.f you start to notice your field of vision getting smaller and it being harder to see things off to the side, see your eye doctor right away,. as loss of peripheral vision can be a sign of glaucoma.
You deserve clear vision. We can help.
With 135+ locations and over 2.5 million procedures performed, our board-certified eye surgeons deliver results you can trust.
Your journey to better vision starts here.
What to Do Immediately After You’re Diagnosed with Glaucoma
Even though you can’t undo damage that may have already occurredand you can’t reverse vision loss, you can slow the progression of glaucoma – or stop it altogether. Blindness only impacts about 5 percent of people suffering from glaucoma. With proper treatment, vision loss from glaucoma can be slowed significantly, or halted altogether.
Treatments for glaucoma work best when started as early as possible. It is important to get regular eye exams to keep track of your eye pressure and ensure that glaucoma is diagnosed as soon as possible.
Be sure to follow all of your doctor’s instructions and explore your options for treatment. To prevent or slow the progression of vision loss, you will need to start taking measures to manage your glaucoma immediately. Swift treatment can help you to keep your vision intact.
The first thing you need to do when diagnosed with glaucoma is to take treatment seriously and act immediately. The longer you put off treatment, the worse things can get, resulting in more vision problems. Encourage your family members to get checked as well since glaucoma can run in families.
How to Manage Glaucoma

In addition to following your doctor’s instructions for treating your glaucoma, implement the following to manage glaucoma:
- Eat a healthy and balanced diet to promote overall health and wellness.
- Exercise regularly to improve blood flow and keep your eye pressure down.
- Take any prescribed glaucoma medication exactly as prescribed.
- Discuss potential side effects or vision changes with your doctor.
- Keep up with regular eye exams.
- Do not smoke. Smoking can irritate and inflame the eyes and cause high blood pressure. If you currently smoke, talk to your doctor about how to quit.
- Minimize your caffeine intake. This can help to keep your eye pressure regulated.
- Sleep with your head elevated to lower eye pressure at night. Try to keep your head above your heart as much as possible.
- Drink fluids slowly to keep your eyes from getting strained.
- Keep your eyes protected. They may be sensitive to light. Further trauma to the eye can increase IOP and exacerbate glaucoma.
Treatments for Glaucoma
There are three main treatments for glaucoma: medications, laser treatment, and surgery. Your doctor will discuss your options with you and help you decide on the best course of action.
Eye Drops for Glaucoma
Prescription eye drops and medications are often the first courses of action, especially for early-stage glaucoma.. Eye drops for glaucoma are designed to either lower the amount of fluid in your eye or help it to drain better. You may be prescribed more than one type of eye drop or medication.
Prescription eye drops for glaucoma include:
- Beta blockers. Medications like Betimol, Timoptic, Istalol (timolol), and Betoptic (betaxolol) reduce production of aqueous humor. They are used once or twice a day.
- Carbonic anhydrase inhibitors. Azopt (brinzolamide) and Trusopt (dorzolamide) lower fluid production in the eye. They are normally given in a twice-daily dosage, but they can sometimes be prescribed for use three times a day.
- Alpha-adrenergic agonists. Lopidine (apraclonidine), Qoliana, and Alphagan P (brimonidine) lower aqueous humor production while also raising fluid outflow. These are used in a twice-daily dosage, but they can sometimes be prescribed for use three times a day.
- Prostaglandin analogs. Zioptan (tafluprost), Xalatan (latanoprost), Vyzulta (latanoprostene bunod), Travatan Z (travoprost), and Lumigan (bimatoprost) increase outflow of aqueous humor in a once-daily dosage.
- Cholinergic or miotic agents. Isopto Carpine (pilocarpine) increases aqueous humor outflow from your eye. It can be dosed up to four times per day.
- Rho kinase inhibitor. Rhopressa (netarsudil) lowers rho kinase enzymes to reduce eye pressure in a once-daily dosage.
- Carbonic anhydrase inhibitors may also be prescribed orally if eye drops alone are not enough to control the pressure in your eyes.
iDose TR: The Newest Treatment Option for Glaucoma
iDose® TR is an innovative, micro-sized implant that provides a continuous release of glaucoma medication directly inside your eye. This advanced technology ensures effective eye pressure control – without the need for daily eye drops.
iDose TR is an excellent treatment option for adults diagnosed with open-angle glaucoma or ocular hypertension who are seeking an alternative to the daily routine of glaucoma eye drops. iDose TR offers a hands-free solution that helps maintain consistent eye pressure without the need for daily intervention, making it ideal for patients who want a more convenient way to manage their glaucoma.
This treatment is particularly suitable for those who have experienced side effects from traditional glaucoma medications, such as eye redness, irritation, or changes in the eye’s appearance.
Since iDose TR delivers medication directly to the eye over time, it significantly reduces the risk of these side effects, allowing patients to manage their glaucoma more comfortably.
Beyond Medications: Laser and Surgical Treatments for Glaucoma

Laser and surgical treatments can help to lower pressure in the eyes. These are often considered after medications are not ineffective or in the case of more advanced glaucoma.
Laser trabeculoplasty
A laser trabeculoplasty for treating open-angle glaucoma creates an opening to allow fluid to drain better out of the eye. This procedure can be done quickly in an office setting and may need to be repeated in the future. You can usually return to your normal activities the next day, but you will need someone to drive you home from the procedure.
After a laser trabeculoplasty, your vision will be blurry.Eye irritation and minor discomfort are common.
It will take up to four to six weeks to know if the procedure is effective. You will likely need to continue medications during this time. In some cases, you may need to continue using medications indefinitely.
Laser Iridotomy
This is a form of laser eye surgery for treating angle-closure glaucoma that creates a small hole in the iris to let the fluid flow properly to the drainage angle. The procedure is quick, and you will likely be able to return to normal activities the next day. You may experience some pain, eye irritation, and blurry vision the day of laser iridotomy.
About a quarter of the time, the drainage angle may not open, and additional measures may need to be taken. You will likely need to continue your glaucoma medications after the procedure as well.
Surgical Trabeculectomy
This surgery creates an opening in the sclera (white part of your eye), and part of the trabecular meshwork where the blockage is occurring is removed to allow for proper drainage. Surgical trabeculectomy is performed in a hospital. You will need to limit your activities for up to a month to allow your eyes time to heal.
Minimally Invasive Glaucoma Surgery (MIGS)
There are several forms of MIGS that are performed to minimize risk by being less invasive than traditional surgery. With MIGS, tiny incisions are made with microscopic instruments. MIGS procedures reduce the risk of complications and shorten recovery times. There are several different types, including:
- Trabeculectomy.
- Shunt placement.
- Laser surgeries.
- Trabecular bypass.
These procedures can be performed for less advanced glaucoma. They usually require less postoperative care.
Surgical Placement of Drainage Tubes
In this procedure, a small shunt is surgically placed in your eye to allow the aqueous humor to drain properly, thereby lowering eye pressure. The surgery typically takes an hour or two, and it is performed in a hospital. It will take two to four weeks before you can fully return to regular activities.
Choosing Surgery for Glaucoma
The treatment your eye doctor recommends will depend on the type of glaucoma you are suffering from, its severity, any other medical conditions you have, and any medications you are taking.
Talk to your health care providers about all possible risk factors and side effects, and be sure they are aware of your full medical history. Generally, your eye care provider will monitor your glaucoma and prescribe a treatment regime to slow its progression. If the condition worsens, they will discuss more invasive treatment measures, like surgery.
You deserve clear vision. We can help.
With 135+ locations and over 2.5 million procedures performed, our board-certified eye surgeons deliver results you can trust.
Your journey to better vision starts here.
References
- Prevalence of Glaucoma Among US Adults in 2022. (November 2024). JAMA Ophthalmology.
- Glaucoma Data and Statistics. (July 2019). National Eye Institute (NEI).
- Glaucoma. MedlinePlus.
- Glaucoma. (2019). American Optometric Association (AOA).
- What Is Glaucoma? (August 2019). American Academy of Ophthalmology (AAO).
- Causes of Glaucoma. (August 2019). American Academy of Ophthalmology (AAO).
- The Genetics of Glaucoma. (October 2017). Glaucoma Research Foundation.
- Understanding Your Glaucoma Diagnosis. (October 2017). Glaucoma Research Foundation.
- Glaucoma Medications. (June 2019). National Eye Institute (NEI).
- Laser Treatment for Glaucoma. (June 2019). National Eye Institute (NEI).
- Laser Iridotomy: 10 Commonly Asked Questions. (July 2019). Glaucoma Research Foundation.
- Glaucoma Surgery. (June 2019). National Eye Institute (NEI).
- What Is MIGS? (September 2019). Glaucoma Research Foundation.

Dr. Salwa Aziz is a board-certified ophthalmologist and fellowship-trained Glaucoma Specialist who specializes in the diagnosis and treatment of simple and complex Cataracts and Glaucoma. Dr. Aziz treats Ocular Hypertension, Primary Open Angle Glaucoma, Narrow Angles, Primary Angle-Closure Glaucoma and Secondary Glaucoma. Dr. Aziz utilizes medical and laser treatments, minimally-invasive glaucoma surgery (MIGS), complex glaucoma surgeries, including Trabeculectomies, Trabeculotomies and Glaucoma Shunt Implants. Dr. Aziz also specializes in vision correction with premium intraocular lens implants and advanced technology cataract surgery.
This content is for informational purposes only. It may have been reviewed by a licensed physician, but is not intended to serve as a substitute for professional medical advice. Always consult your healthcare provider with any health concerns. For more, read our Privacy Policy and Editorial Policy.