Retinopathy Guide: Diabetic, Other Types & Treatment
Home /
Last Updated:
Table of Contents
The retina, at the back of your eye, is partially responsible for transmitting light into your brain to create images of the world. When something happens to your retina, you can experience blurry vision, headaches, or vision loss because of retinopathy.
There are a few types of retinopathy, some of which are associated with specific medical conditions that you can manage with a physician as well as your eye doctor. Getting routine eye exams as often as needed, depending on your overall health, will help you get an early diagnosis if you develop retinopathy. You can then follow a treatment plan and mitigate damage to the eye.
What Is Retinopathy? Should I Be Worried About It?
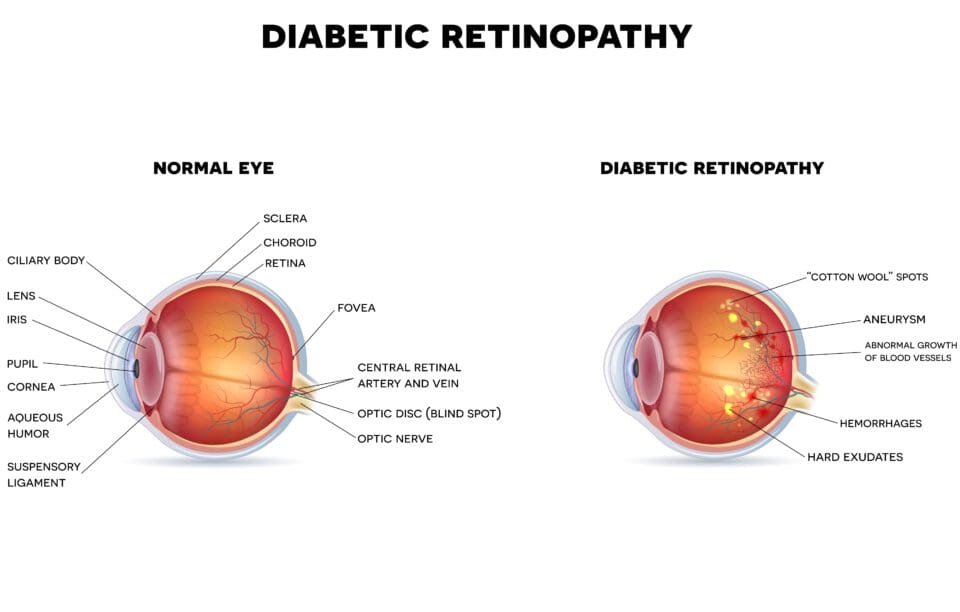
The retina is part of your eye involved in processing light into images. This layer of nerves sits at the back of the eye, sensing light with specialized cells called rods and cones. These cells are located in an area called the macula.
The cornea and the lens of your eye help to focus light onto the retina, through the pupil. Once cells on the retina detect colors and light or darkness, the sensations are sent through the optic nerve to the brain, where the images are processed so you can see.
You deserve clear vision. We can help.
With 135+ locations and over 2.5 million procedures performed, our board-certified eye surgeons deliver results you can trust.
Your journey to better vision starts here.
Unfortunately, several conditions can affect your retina’s health, which might cause vision problems and vision loss. The retina has its own blood vessels. In a healthy retina, the blood vessels grow around the retina and bring it oxygen and nutrients. In an unhealthy retina, blood vessels may split and leak blood, grow over the retina and macula, or grow through the layers, which can cause vision problems. Without enough nutrients or under high pressure, the retina may detach or deteriorate, which can eventually lead to blindness.
The term retinopathy covers several diseases that damage the retina. The most widely known of these is diabetic retinopathy, but other conditions can lead to damage to this vital part of your eye. It is important to get regular eye exams so your optometrist or ophthalmologist can note changes in your vision like floaters or lower visual acuity, which might indicate the beginning of a type of retinopathy.
Early diagnosis helps you get the care you need to keep your vision stable as long as possible.
Types of Retinopathy
There are several types of retinopathy, with different symptoms and underlying causes. It is important to understand what caused retinopathy, so you understand how to approach treatment and management of the condition. Regardless of the type, however, it is vital to work with your ophthalmologist or optometrist to monitor the condition’s progress.
Diabetic retinopathy: People with either type 1 or type 2 diabetes are at risk for diabetic retinopathy, one of the most common forms of retinopathy. This is a slow, progressive disease that can take years to develop.
Managing your diabetes with your physician’s help is the best prevention and treatment for diabetic retinopathy. If you develop the condition, you may need additional treatment and monitoring.
There are two basic forms of diabetic retinopathy.
- Proliferative retinopathy: New blood vessels form, but they are unstable, with weak walls, so they may leak fluid or blood. They grow over the retina, which can lead to vision loss.
- Between new blood vessels forming over sensitive cells and fluid leaking into the area, your retina will become irritated, which can lead to scar tissue. This condition can also lead to retinal detachment.
- Non-proliferative retinopathy: Blood vessels in the retina deteriorate, and then become blocked and deformed. Proteins, fluids, and fats leak out of these vessels and collect in the retina. This causes swelling, which leads to poor visual acuity, or blurry vision.
Symptoms of diabetic retinopathy may include:
- Blurry vision
- Sudden vision loss in one or both eyes
- Black spots
- Flashing lights
- Trouble reading, seeing detailed work, or seeing other things up close
People who have either type of diabetes need regular vision checkups. An ophthalmologist examines the inside of your eye, including your retina using an ophthalmoscope. They may use a dye during this exam so they can see leaking blood vessels.
The best treatment and prevention for diabetic retinopathy is controlling your blood sugar. If you develop proliferative diabetic retinopathy, you may need specific vision treatments, including:
- Laser therapy, or photocoagulation, which creates intentional scar tissue areas to slow down the growth of blood vessels.
- Anti-vascular endothelial growth factor (anti-VEGF) drugs, which can stop fluid leaking from damaged blood vessels.
- Surgically reattaching the retina if it detaches.
- Removing all or part of the vitreous humor (vitrectomy) to reduce floaters.
- Corticosteroid injections.
Retinopathy of prematurity (ROP): This form of retinopathy occurs in premature babies. Children born too early or at a low birth weight are at risk of blood vessels around the retina not forming fully.
About 3.9 million infants are born in the United States every year; between 14,000 and 16,000 of those babies are at risk for ROP. The symptoms in the early stages of ROP are subtle. As the condition advances, the retina can become detached and the child can go blind.
Babies with low birthweight or who are born prematurely can be screened for ROP if:
- They are born prior to 36 weeks
- They weigh less than 4 pounds, 6 ounces at birth
If the child gets too much oxygen or not enough oxygen right after birth, they may develop ROP. Oxygen levels are closely monitored and adjusted, but an ophthalmologist can also examine your baby to diagnose potential retinopathy.
An ophthalmologist should examine infants who are at risk before they leave the hospital. Then, they should be examined again at 8 weeks old.
Only an experienced pediatric ophthalmologist can identify ROP in children. Even a healthy baby’s vision will be poor for the first several months, as the eyes and brain develop. An experienced ophthalmologist can examine the inside of your child’s eyes for symptoms of retinopathy.
Children with active retinopathy should receive eye exams every one to two weeks until they are 14 weeks old. Then, they should be examined every one to two months.
Typically, this condition gets better on its own. Abnormal blood vessels, which can grow in or around the retina, may disappear. Diagnosing the condition is important, and monitoring it for changes is also important. If the baby needs treatment, they get it in the first few months of life. The pediatric ophthalmologist will be able to tell, based on improvement and treatment, if there is significant damage to vision.
Children who have ROP are at risk of:
- Retinal detachment
- Cataracts
- Crossed eyes
- Glaucoma
- Lazy eye
- Nearsightedness
Treatment may include vascular endothelial growth factor (VEGF) inhibitors, which are common medications to treat retinopathy in adults too. Sometimes, laser treatments are used to destroy unhealthy blood vessels. An older surgery called cryotherapy can use cold to destroy these blood vessels. Detached retinas may be reattached.
In more severe cases of ROP, a scleral buckle (a silicon band around the eye) can keep the retina in place after it is reattached. This can keep the back of the eye flat.
Hypertensive retinopathy: Cardiac hypertension, or high blood pressure, damages blood vessels throughout the body. This includes the blood vessels around the retina, which can cause hypertensive retinopathy.
Abnormalities that can damage the retina include thickening of the small arteries, blockages in the retinal blood vessels, and bleeding from thinned or damaged blood vessels. Leaking blood or fluid can cause floaters in the eyes and blurred vision, but other than these issues, there are few early symptoms of this condition. Later symptoms of hypertensive retinopathy can include vision loss, double or cloudy vision, and headaches.
An ophthalmologist or physician will diagnose this condition by looking at your eyes with an ophthalmoscope. They use this device to look for white areas on the retina, which are pale because they are not getting enough blood. Other signs of hypertensive retinopathy may be bleeding areas from ruptured blood vessels or swelling underneath the retina or near the optic nerve.
In rare cases, swelling of the optic nerve from leaked blood can cause sudden vision loss, which requires emergency treatment in the hospital.
Hypertensive retinopathy is directly caused by cardiac hypertension, so lowering your blood pressure is the best treatment or prevention. This may include following your physician’s instructions to:
- Maintain a healthy body weight.
- Exercise regularly.
- Eat less salt, and more fruits and vegetables.
- Get regular checkups, both with your physician and with your optometrist.
- Take blood pressure medications, if prescribed.
Many of the symptoms of hypertensive retinopathy can clear up when you manage your blood pressure. Some damage may remain, so you may need corrective wear like glasses to improve your visual acuity. You may still have areas of vision loss.
Central serous chorioretinopathy (CSCR): While other types of retinopathy have specific causes, central serous chorioretinopathy is idiopathic, meaning it begins for unknown reasons. Fluid accumulates in the membrane behind the retina, seeping in between the layers and causing them to separate.
Some potential causes of CSCR include:
- High blood pressure.
- Drinking too much caffeine on a regular basis.
- Corticosteroid treatment.
The main symptoms of CSCR are blurry vision and poor night vision. These may occur suddenly or shift throughout the day. Other symptoms include:
- Blind spots
- Distorted shapes
- Reduced visual sharpness

An optometrist or ophthalmologist can diagnose CSCR using an ophthalmoscope to examine the buildup of fluid in or around the retina. This fluid may look like bubbles.
Even if your vision is impacted by central serous chorioretinopathy, most cases resolve within three to four months entirely on their own. It may be an uncomfortable problem during that time, but your eye doctor will monitor changes and note when fluid begins receding. Full vision is often restored after six months, with no treatment or intervention required.
In rare cases, you may have some lasting symptoms like:
- Distortion in your vision
- Decreased contrast sensitivity
- Difficulty seeing at night
If you take corticosteroids for another condition, you may need to work with your physician to reduce or stop taking the medication to manage your vision’s health. However, you should not adjust the dose of any prescription drugs you take without consulting your doctor first.
Sometimes, persistent CSCR requires interventions like photodynamic therapy, which uses a combination of light and a chemical substance that makes some cells sensitive to light. About half of people who are affected by CSCR once will experience the condition again, but it will often clear up after a few months.
Management & Treatment Require Regular Eye Exams
If you are diagnosed with any type of retinopathy, work with your eye doctor and your physician to manage the condition. Regular eye exams will help your eye doctor determine if you have any risk of retinopathy or if vision problems are symptoms of retinopathy.
If you suffer from sudden blurry vision, spots in your vision, flashes of light, blind spots, distortion, or have trouble reading or doing up-close work, you should schedule a doctor’s visit to check on these vision problems.
You deserve clear vision. We can help.
With 135+ locations and over 2.5 million procedures performed, our board-certified eye surgeons deliver results you can trust.
Your journey to better vision starts here.
References
- Medical Definition of Retina. (December 2018). MedicineNet.
- What Is the Retina? VRM Institute.
- Retinopathy: What Is It? (August 2017). Harvard Health Publishing, Harvard Medical School.
- Diabetic Retinopathy. American Optometric Association (AOA).
- Diabetic Retinopathy. (August 2019). National Eye Institute (NEI).
- Retinopathy of Prematurity. (July 2019). National Eye Institute (NEI).
- Hypertensive Retinopathy. (January 2020). Ada Health.
- Hypertensive Retinopathy Revisited: Some Answers, More Questions. (2005). British Journal of Ophthalmology (BMO), British Medical Journal (BMJ).
- Central Serous Chorioretinopathy. (June 2019). Medscape.
- CSCR: Diagnosis and Treatment. (July 2014). Review of Ophthalmology.
This content is for informational purposes only. It may have been reviewed by a licensed physician, but is not intended to serve as a substitute for professional medical advice. Always consult your healthcare provider with any health concerns. For more, read our Privacy Policy and Editorial Policy.