Does Keratoconus Ever Lead to Blindness?
Home / Keratoconus: Signs, Timelines & Treatments /
Last Updated:
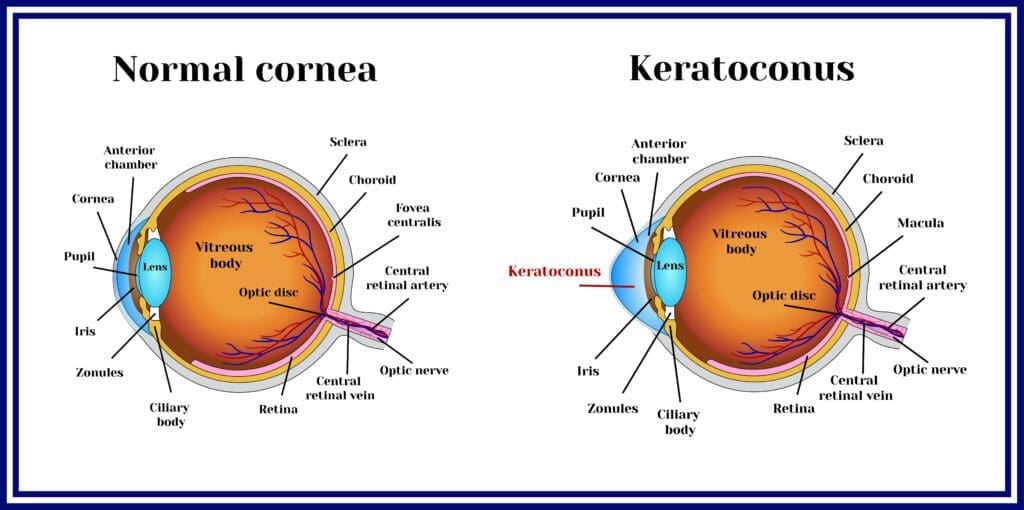
Keratoconus is an eye condition that causes your cornea to thin out and become cone-shaped, leading to vision distortion related to a misshapen and bulging cornea. Keratoconus is a degenerative disorder that ranges from mild to severe. It is a progressive condition.
Table of Contents
Keratoconus starts out mild and usually progresses slowly over a period of several years. Without treatment, keratoconus can continue to progress. Vision can move from blurry to distorted, and it can become significantly impaired. Keratoconus rarely leads to complete blindness, although the progression of the disorder can’t be undone.
Keratoconus can be managed to keep vision stable. Treatments for keratoconus, such as specialized contact lenses, Intacs, collagen cross-linking, and corneal transplants, can all be beneficial. To avoid vision loss, proper treatment should begin as soon as possible once symptoms start.
What Is Keratoconus?
Your cornea is the clear dome-shaped outer covering of your eye. It is responsible for focusing light onto your retina.
Keratoconus is when the cornea thins out and bulges into a cone shape. This causes light rays to be focused improperly, making your vision blurry and distorted.
You deserve clear vision. We can help.
With 135+ locations and over 2.5 million procedures performed, our board-certified eye surgeons deliver results you can trust.
Your journey to better vision starts here.
Keratoconus is a progressive and degenerative condition that will continue to worsen over time without intervention. The condition can occur in one eye or both, and it’s worsened by rubbing your eyes.
Symptoms include:
- Blurry vision.
- Eye redness and/or swelling.
- Light sensitivity.
- Distorted vision (lines appearing wavy or bent instead of straight).
- Nearsightedness and/or astigmatism.
Progression of Keratoconus
Keratoconus typically progresses slowly over a period of several years. Sudden swelling can lead to corneal scarring, which can worsen the condition more quickly.
In the early stages of the condition, your eyesight can appear blurry and slightly distorted. As keratoconus progresses, your cornea thins out more, and the cone-shaped bulge worsens. Your vision will continue to deteriorate.
Keratoconus Stages & Timelines

Keratoconus usually starts in the late teens and progresses over a period of 10 to 20 years until the corneal shape stabilizes, the U.S. National Library of Medicine (NLM) reports.
In its early stage, blurry vision and sensitivity to light are common. The cornea will continue to thin out and get more misshapen slowly over a period of years, and symptoms will get worse.
Keratoconus does not always impact each eye equally. It can progress more quickly in one than the other, and it can get worse in one eye and not the other. Keratoconus can cause your vision to be different from eye to eye, and symptoms can be very different in each eye.
Late-stage, or advanced, keratoconus can cause an irregular astigmatism, leading to nearsightedness, significant vision distortion and even loss of vision.
Most of the time, keratoconus progresses slowly, but it can swell abruptly and then scar. This can mean a much faster progression of the disorder.
You deserve clear vision. We can help.
With 135+ locations and over 2.5 million procedures performed, our board-certified eye surgeons deliver results you can trust.
Your journey to better vision starts here.
Side Effects of Untreated Keratoconus
Someone with keratoconus can expect a handful of side effects over time, especially if the condition progresses. Without treatment, you are likely to experience a thinning cornea or a bulging cornea. Both are irreversible.
You may not go blind, but your vision will get worse, and you likely will have increase eye pain over time.
Corneal scarring is another potential side effect. The condition, which impacts the cornea so severely, makes it impossible for patients to wear contact lenses. Even eyeglasses will provide minimal help over time.
Riboflavin 5-Phosphate is the only FDA-approved prescription medication for keratoconus. Sold under brand names Photrexa and Photrexa Viscous, it comes in the form of drops and should only be taken under the close care of a doctor.
The leading side effect from the drops is a higher-than-normal sensitivity normal to light. Many people who use the drops, which are known as photo enhancers, keep a pair of sunglasses handy at all times.
Other known side effects include hazy vision and blurry vision, dry eye and sensations of having a foreign object in the eye(s). A small number of patients report an increased number of headaches.
Treatment Options for Keratoconus
The best treatment for keratoconus depends on the stage and progression of the disorder.

Early on, blurry vision and nearsightedness can be managed with prescription eyewear. Later, keratoconus can be treated by your ophthalmologist with a variety of procedures, including a full surgical transplant of the damaged cornea, in extreme cases.
- Eyeglasses and soft contact lenses: With mild keratoconus, prescription eyeglasses or soft contacts can correct your blurry and distorted vision. Glasses and contacts will not stop the progression of the disorder, however.
You will need to continue to get your eyes checked on a regular basis, so your eye doctor can keep up with the progression. You will likely need to continue to get new and revised prescriptions to keep up with your changing vision. - Rigid gas permeable contact lenses: These are specialized contacts that can be specifically fitted to the shape of your eye. They correct vision related problems to keratoconus once soft lenses and eyeglasses are insufficient.
- Specialized contact lenses: Hard and soft contact lenses can be “piggybacked,” or placed on top of each other, to treat keratoconus. Hybrid lenses that are hard in the middle and soft on the outer ring, for a more comfortable fit, are also an option.
Scleral lenses are a type of contact lens that vault over the cornea without touching it. These lenses can be beneficial in treating vision issues related to keratoconus as well. - Intacs: These are corneal implants that are surgically placed into your eyes to flatten and reshape your cornea. They are used to treat astigmatism and myopia related to keratoconus.
These ophthalmic medical devices can reduce the cone shape of your cornea, which is caused by keratoconus. Intacs can even help to potentially defer the need for a full corneal transplant. - Collagen cross-linking: This procedure can be done by an ophthalmologist. It uses eye drops and a special UV light to make your cornea stronger and keep it from bulging any further.
- Corneal transplant: When keratoconus is advanced and the cornea is significantly damaged, a surgery to replace the diseased cornea with a strong donor cornea can be done by an ophthalmologist. Corneal transplants are for severe cases of keratoconus. They can help to restore vision through a surgery called a keratoplasty.
Regular eye exams can help to detect keratoconus early. Your doctor will keep track of the shape of your cornea and any changes in your vision. Iron deposits on your cornea can also be an indicator of the disorder that your eye doctor can monitor.
Try to avoid rubbing your eyes. This can put you at risk for keratoconus and increase its severity. Eye rubbing thins your cornea and can cause scarring.
The good news is that keratoconus can be managed. You can help to at least slow its progression if you take good care of your eyes.
Catching the disorder as early as possible and beginning treatment can help to preserve your vision. Early diagnosis and intervention are the best ways to prevent vision loss and damage to your eyes as a result of keratoconus.
Helpful Resources for People with Low Vision
A number of national non-profits exist to help people who live with low vision. All can be helpful, though most differentiate by their core audience (seniors, children, fully blind, etc.).
National Support Groups
American Council for the Blind: This is a consumer organization that helps its visually impaired members maintain security and independence.
American Diabetes Association: The ADA is a network of volunteers, caregivers and healthcare professionals that educates people about diabetes, a leading cause of adult blindness, and provides resources to those in need.
American Foundation for the Blind: The foundation advocates for people who are losing their vision, particularly older Americans. It also works with companies to design and refine products for customers who are vision-impaired.
Glaucoma Research Foundation: This non-profit is dedicated to finding a cure for glaucoma, and it funds worldwide glaucoma research. The foundation is a good resource for people who are learning to live with glaucoma.
Helen Keller International: This group is dedicated to saving the lives and sight of the most vulnerable.
National Federation of the Blind: The federation has a large network of blind members that provides programs, services and resources to people who need help. This is a diverse community of people helping one another.
National Industries for the Blind: NIB is the largest employer of blind people in the country. It’s also an employment resource as well as an agency that creates opportunities for people who are blind but still want to work.
You deserve clear vision. We can help.
With 135+ locations and over 2.5 million procedures performed, our board-certified eye surgeons deliver results you can trust.
Your journey to better vision starts here.
References
- What Is Keratoconus? (December 2019). American Academy of Ophthalmology (AAO).
- Keratoconus Symptoms. (December 2019). American Academy of Ophthalmology (AAO).
- Keratoconus. (January 2020). U.S. National Library of Medicine (NLM).
- Keratoconus. (2020). American Optometric Association (AOA).
- Keratoconus Diagnosis and Treatment. (December 2019). American Academy of Ophthalmology (AAO).
- About Intacs. (2015). Addition Technology, Inc.
- Keratoconus: Know the Signs of This Mysterious Eye Disease. (February 2018). Cleveland Clinic.
- Keratoconus. (August 2021). National Organization for Rare Disorders. Date fetched: August 6, 2021.
- Keratoconus Medication. (October 17, 2018). Medscape. Date fetched: August 6, 2021.
This content is for informational purposes only. It may have been reviewed by a licensed physician, but is not intended to serve as a substitute for professional medical advice. Always consult your healthcare provider with any health concerns. For more, read our Privacy Policy and Editorial Policy.
