Intacs for Keratoconus: What to Know
Home / Keratoconus: Signs, Timelines & Treatments /
Last Updated:
Table of Contents
Intacs are brand-name medical devices that are surgically placed into your eyes to reshape your cornea and treat keratoconus.
Keratoconus is a condition that causes your cornea to thin out and become irregularly shaped (like a cone). The condition is both progressive and degenerative.
Vision distortion from keratoconus can be treated with contact lenses and glasses to a point. As the condition progresses, more intensive treatment is needed.
Intacs can actually help to stall the progression of the disorder and reshape your cornea. Intacs can potentially defer your need for a corneal transplant, but Intacs still involve a surgery that carries some risk.
The placement of Intacs is a quick surgical procedure done in an outpatient surgical center or an ophthalmologist’s office. It comes with a fast recovery time.
Intacs Corneal Implants
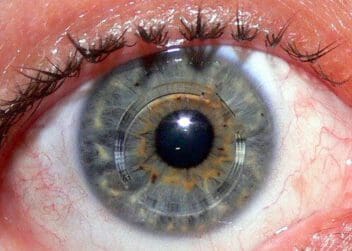
Intacs were initially designed to be used for refractive eye surgery to correct for myopia (nearsightedness). They are medical ophthalmic devices that are surgically placed into your eyes. In 2004, the FDA approved the use of Intacs for the treatment of keratoconus.
Intacs are a brand-name product. They consist of a thin clear plastic ring that is surgically placed into the middle of your cornea.
You deserve clear vision. We can help.
With 135+ locations and over 2.5 million procedures performed, our board-certified eye surgeons deliver results you can trust.
Your journey to better vision starts here.
With keratoconus, your cornea develops a cone shape as it thins out and bulges outward. This can distort your vision due to changing the way light is reflected back onto the retina. Intacs can help to flatten the cone and therefore improve your vision.
Keratoconus is a progressive disorder. It usually starts in a person’s late teens. Over the next 10 to 20 years, it can continually progress until vision is significantly impaired. Eventually, it can result in the need for a corneal transplant.
Intacs is a much less invasive surgical procedure that can potentially slow the progression of keratoconus. Placement of Intacs can at least delay your need for a corneal transplant.
Intacs & Other Keratoconus Treatments
There are varying degrees of keratoconus, and different treatment needs for the various stages.
With mild keratoconus, in the early stages, blurry vision, sensitivity to light, and some vision distortion are common. As the cornea thins and continues to bulge through the progression of the disorder, vision becomes more and more impaired.
Treatment options for keratoconus typically progress like this:

- Eyeglasses or soft contacts
- Rigid gas permeable contacts (or potentially hybrid or “piggybacking contacts”)
- Intacs
- Collagen cross-linking
- Corneal transplant
At first, eyeglasses or standard soft contact lenses are often enough to correct for the vision issues related to keratoconus. As the disorder progresses, however, specialized contacts are often needed.
Keratoconus can deteriorate the cornea to the point where contacts are not comfortable to wear anymore. Prescription contacts and eyeglasses also do not slow the progression of keratoconus. Deterioration of the cornea is not reversible.
Intacs can help to reshape the cornea, flatten the cone, and minimize the risk for disease progression and the need for a corneal transplant.
Collagen cross-linking is another procedure an ophthalmologist can perform to strengthen the cornea. This can stabilize it and keep keratoconus from progressing further. Corneal cross-linking does not reshape the cornea; instead, it serves to stabilize it.
These two procedures (Intacs and corneal cross-linking) can complement each other. The cross-linking can stabilize the cornea, while Intacs reshape it.
A corneal transplant is the most extreme treatment for keratoconus. It can be necessary when the disorder has progressed to an advanced stage, and vision is severely impaired. A corneal transplant is a surgical procedure that replaces the diseased cornea with a healthy donor cornea.
Pros & Cons of Intacs
As opposed to contact lenses and prescription eyeglasses, Intacs can reshape your cornea to restore vision loss attributed to keratoconus. Progression of the disorder can also be slowed.
The Intacs procedure is reversible, and the inserts can be removed if necessary.
The procedure to place Intacs is minimally invasive, and recovery is usually fairly quick. The placement of Intacs can also make it so that you can comfortably wear contacts again.
Just as with any surgery, there is a risk of complications with Intacs, such as infection. You may also experience glares or halos around lights, as well as some difficulties with night vision.
Intacs can improve your vision, but blurriness and vision distortion are possible after the procedure. This can mean that you will need to continue to wear prescription glasses or contacts.
What to Expect With Intacs
Keratoconus can be diagnosed through regular eye exams that measure the shape of your cornea as well as any vision issues. By detailing changes with routine eye exams, an eye doctor can recognize keratoconus in the early stages. Early diagnosis allows your doctor to provide you with the best treatment options.
Keratoconus usually progresses very slowly over a period of years, but it can differ in its progression from eye to eye.
The first line of treatment is generally prescription eyewear. Once that is no longer successful and the condition is more advanced, procedures such as Intacs may be recommended.
You deserve clear vision. We can help.
With 135+ locations and over 2.5 million procedures performed, our board-certified eye surgeons deliver results you can trust.
Your journey to better vision starts here.
The Procedure
Prior to Surgery
Before Intacs are placed into your eyes, your eye doctor will perform a full eye exam and measure the size and shape of your corneas. They will discuss the treatment, procedure, and recovery information with you in depth.
During the Intacs Surgical Procedure
During the actual procedure, topical anesthesia is used to numb your eyes. You will have the surgery done in an ophthalmologist’s office or an outpatient surgery center. It typically only takes about 15 to 20 minutes to complete the full procedure.
The surgeon will make a small incision, usually with a laser, in the surface of the cornea. To stabilize the eye, a centering guide is placed on the eye, and the corneal layers are separated.
The Intacs are placed on the outer edge of your cornea to smooth and flatten it. You can feel pressure and a small tugging sensation as the outer suture is placed.
Post-Procedure Recovery
Depending on the level of correction needed, you may need to wear contact lenses or glasses to see clearly in the first few days after surgery. The American Academy of Ophthalmology (AAO) reports that minor stinging and some tearing are common right after the placement of Intacs. The relatively minor discomfort should be manageable with over-the-counter painkillers.
Intacs are a safe and minimally invasive treatment for keratoconus that can help to slow the progression of the disorder. The treatment can improve your vision and defer the need for a more invasive corneal transplant and severe vision deterioration.
You will need someone to drive you home from the doctor’s office after you have your procedure. In addition, you should plan on not driving or lifting heavy objects for one or two days. When prepping for surgery, you should consider stocking your fridge with some easy-to-eat foods for meals right after surgery.
Prior to the procedure, your doctor will go review with you the exact recovery procedures, and the doctor’s office will and schedule follow-up appointments.
As you begin the initial stages of recovery, you may feel like you have a foreign object in your eye for a few days. Don’t worry. The sensation is temporary. It will abate in a few days, and your eye will feel normal again.
Risks Factors Associated with Keratoconus
No one knows what causes keratoconus, but the following factors can increase your chances of developing the condition:
- Family history: You will probably develop keratoconus if it is present in other family members. The same applies if they have systemic disorders like Down syndrome. Statistics show 1 in 10 people with keratoconus has at least one parent with the condition. Regular eye check-ups will diagnose and arrest it early.
- Eye rubbing: Rubbing your eyes continuously and vigorously may be a sign that keratoconus is progressing. Visit an ophthalmologist to rule it out.
- Eye inflammation: Frequent swelling caused by allergies or irritants will damage the corneal tissue, leading to the disease. Getting treatment for underlying allergies will protect your eyes from developing keratoconus.
- Age: Doctors are likely to discover it during the teenage years. Younger patients may need surgical intervention as the disease progresses.
- Asthma, hay fever, retinitis pigmentosa, sleep apnea, floppy eyelid syndrome, connective tissue disorder, and Ehlers-Danlos syndrome: These medical conditions are possible factors for developing keratoconus.
Identifying the risk factors early enough helps in preventing and managing the condition.
You deserve clear vision. We can help.
With 135+ locations and over 2.5 million procedures performed, our board-certified eye surgeons deliver results you can trust.
Your journey to better vision starts here.
References
- About Intacs. (2015). Addition Technology, Inc.
- Intacs Surgery for Keratoconus. National Keratoconus Foundation (NKF).
- Keratoconus. (January 2020). U.S. National Library of Medicine (NLM).
- Examining the Cross-Linking/Intacs Link. (November 2012). Review of Ophthalmology.
- How Painful Is Recovery From Intacs Surgery? (October 2015). American Academy of Ophthalmology (AAO).
- Keratoconus. (March 2021). Mayo Clinic.
- Keratoconus. (May 2021). American Academy of Ophthalmology.
This content is for informational purposes only. It may have been reviewed by a licensed physician, but is not intended to serve as a substitute for professional medical advice. Always consult your healthcare provider with any health concerns. For more, read our Privacy Policy and Editorial Policy.