Trabeculectomy Surgery: Risks, Recovery & How It Works
Last Updated:
Glaucoma is associated with high fluid pressure that can damage the optic nerve, so finding a way to lower intraocular pressure is important. Eye drops and laser surgery may be used first, but if these do not work, your ophthalmologist may recommend trabeculectomy.
Table of Contents
This operation creates a bleb in the sclera, or white part of your eye. This is like a small pocket that collects some of the aqueous fluid in your eye to relieve pressure. Fluid that collects in the bleb will be naturally absorbed into other surrounding tissues in your eye.
This successful surgical procedure requires consistent visits to your ophthalmologist over several weeks, to ensure you heal well, the fluid pressure in your eye lowers, and you maintain your vision. It is important to be patient as you recover from trabeculectomy, but report any symptoms that are out of the ordinary.
There are risks to this surgery, as with any medical procedure. If your ophthalmologist determines that trabeculectomy is necessary, the benefits outweigh the costs and risks.
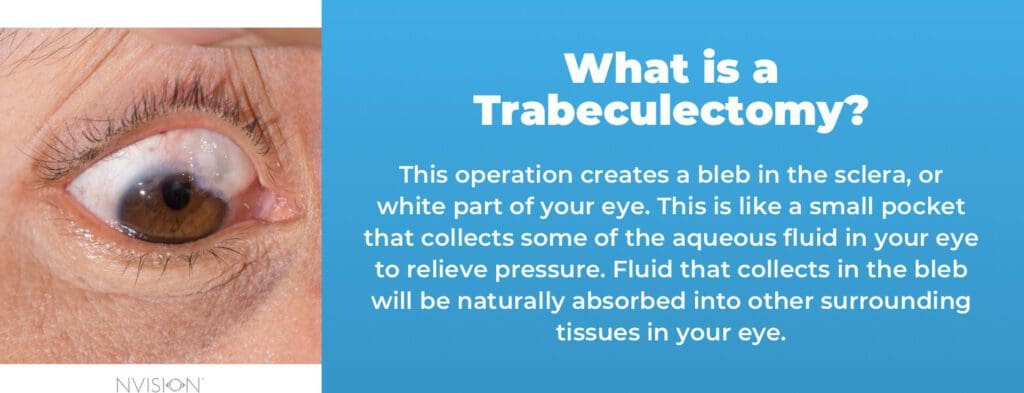
What is Trabeculectomy?
Trabeculectomy is a standard surgical procedure used to treat glaucoma. The end goal of the procedure is to reduce intraocular pressure in situations where laser surgery and medical treatments have failed.
Trabeculectomy involves creating a new channel called a bleb, which allows smooth drainage of aqueous humor from the eye. During the surgery, a hole is made in the sclera to allow fluid to drain from the eye. Fluid from the eye is then shunted, bypassing the blocked trabecular meshwork.
You deserve clear vision. We can help.
With 135+ locations and over 2.5 million procedures performed, our board-certified eye surgeons deliver results you can trust.
Your journey to better vision starts here.
Restoring the eye’s drainage ability lowers the intraocular pressure. While it won’t treat glaucoma-related vision loss present before, it prevents or slows progressive vision loss.
Operating the trabecular meshwork is a delicate procedure and should be done in a sterile operating room. Trabeculectomy can successfully control eye pressure for five years in about 60-80% of patients.
When Trabeculectomy Becomes Necessary
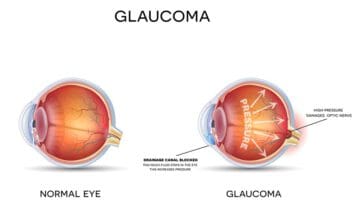
Glaucoma is a term covering several conditions that damage your optic nerve, leading to progressive peripheral vision loss. Most glaucoma conditions are associated with high fluid pressure in the eye.
Sometimes, these problems are severe, as in angle-closure glaucoma, which happens rapidly and is considered a medical emergency. Most types of glaucoma are primary open-angle glaucoma, which is a chronic, progressive condition.
Damage to the optic nerve is permanent, so it is important to get regular eye exams so your optometrist or ophthalmologist can detect high fluid pressure before it becomes a serious problem. While you cannot stop glaucoma, you can slow its progression with appropriate treatment. Typical treatment plans involve eye drops and monitoring fluid pressure, but your eye doctor may recommend surgery.
There are several types of glaucoma surgery, ranging from laser procedures to incision surgeries. Trabeculectomy is one of the more intensive surgical procedures, so your ophthalmologist will likely try other methods of managing your fluid pressure first. Still, this is an important surgical option to treat glaucoma, and many people successfully undergo this operation.
The Trabeculectomy Surgical Procedure

In the days before your trabeculectomy, you will be asked to stop using any eye drops, including those associated with lowering fluid pressure in your eye. Typically, you can expect your surgery and recovery timeline to look like this:
Day of Surgery
You will be asked to stop taking any medications, like drops or tablets. You should also avoid taking any over-the-counter painkillers like aspirin, along with blood thinners like warfarin, because these can have an adverse interaction with the procedure and your healing process afterward.
During the Surgery
You may receive mitomycin C. This is a drug originally developed to treat cancer, but it is now used after glaucoma surgery to reduce scarring. By preventing scarring around the bleb, your eye will be able to drain better, so you have healthier fluid pressure. Mitomycin C will only be applied during the surgery and then washed off with sterile water. You will not be responsible for applying it or removing it.
You can undergo this operation with either local anesthesia or under general anesthesia. If you choose to have general anesthesia, you will need to have an overall physical assessment with a physician to ensure your health. Many people do undergo this surgery with only local anesthesia and light sedation. Either way, once the procedure is complete, you will be sent home the same day.
Trabeculectomies typically take between 45 and 60 minutes.
Day After Surgery
You can spend time in a recovery room after the procedure, ensuring that your eye is stable and allowing time for sedation or the anesthesia to wear off. Then, you can go home. Be sure to get someone to drive you as you will not be able to drive safely. You will wear a clear eye patch, pad, or shield to protect your eye for a day after the trabeculectomy. Your eye surgeon or doctor will remove it the next day when you have your first postoperative exam, but you will need to keep wearing a shield at night and for some activities. After your first eye exam, your ophthalmologist will want to see you once a week for up to a month.
Two to Three Weeks After Surgery
Your ophthalmologist will tell you when you can stop wearing a shield at night, but you’ll generally be advised to keep wearing it for two to three weeks. Your vision may be blurry for the first few weeks after the operation, but you should notice improvement after two or three weeks too. Your eye may be sore during this time, in part because of the surgical sutures. These will not be the type of sutures that dissolve, so you must return to your ophthalmologist to have them removed after two to three weeks. This takes a few minutes, and you will receive a local anesthetic for your eye.
Two to Three Months After Surgery
Your eye should be mostly healed, and your vision should stabilize. Although you will not recover any vision lost from glaucoma damage, you should have a similar level of visual acuity as before your operation.
You deserve clear vision. We can help.
With 135+ locations and over 2.5 million procedures performed, our board-certified eye surgeons deliver results you can trust.
Your journey to better vision starts here.
Trabeculectomy Recovery & Risks
Immediately after trabeculectomy, your eye will be red and swollen. This is normal, and it should go away over a few weeks or months.
During this healing time, you will have regular appointments with your eye doctor. They will watch the healing process and ensure the redness, swelling, and eyelid drooping go away. If they do not resolve, there will be further steps; however, this is rare.
You should not feel the drainage bleb, even if you can lift your eyelid and see it. If you can feel it or there is some discomfort in the area of the bleb, you can talk to your ophthalmologist about potential remedies.
You will need to avoid some activities for several weeks after trabeculectomy, including:
- Strenuous exercise like jogging.
- Swimming.
- Contact sports like football.
- Bowing your head too low, such as in yoga.
- Being upside down.

You may also need to take up to two weeks off work or school to ensure your eye has healed. After your first eye exam the day after your surgery, you should be able to safely read, watch television, or use your eyes for similar activities.
It is safe to fly within two weeks after the surgery but missing your weekly eye exams could be detrimental. If your eye is reasonably healthy, and you must fly for work or a personal matter, talk to your ophthalmologist about how to manage your healing process.
There are risks to any type of surgery, including trabeculectomies. Complications from this operation are extremely rare, but the most serious one is a sudden drop to very low fluid pressure in the eye.
An abrupt drop in your eye’s fluid pressure will be associated with discomfort, pain, and sudden vision changes like blurry or cloudy vision. Report these issues to your surgeon for help.
- Infection and inflammation.
- Bleeding.
- Blurry or distorted vision.
- Vision loss.
- Scarring on the eye.
- You are at a slightly higher risk of developing cataracts after this procedure. You could also develop astigmatism, which is manageable with glasses or contact lenses.
Alternatives to Trabeculectomy
While a trabeculectomy is the gold-standard surgery for lowering intraocular pressure for glaucoma patients, it does have drawbacks and failures. Other surgical procedures include minimally invasive glaucoma surgery, canaloplasty, and trabectome.
Apart from surgery, other methods of controlling IOP with few complications include:
- Medications. Glaucoma can be treated using topical medications that lower IOP. These drugs reduce eye pressure by stimulating the drainage of aqueous humor from the eye.
- Perfusion pressure. This treatment option relies on the difference between IOP and blood pressure. According to research studies, proponents of this treatment claim that low blood pressure can lead to low ocular perfusion pressure.
- Meditation. Patients with glaucoma can also benefit from mindful meditation. Meditation is thought to lower IOP by 4mm Hg.
- Ginkgo. This herbal plant is drawn from leaves of the Ginkgo tree, which has been used as a Chinese drug for more than 5000 years. The plant contains flavonoids, cyanidin, and lactones, which are all antioxidants and inhibits apoptosis.
Trabeculectomy Success Rates
Trabeculectomy requires an incision in the sclera, or white part of your eye, to create a tiny flap. Then, the surgeon will create a small bubble or pocket in the conjunctiva, which is the clear coating over your sclera. This bubble is called a filtration bleb.
Typically, the bleb hides under your eyelid so it will not be seen when someone looks at you, but this new pocket allows aqueous humor to drain out of your eye at a healthier rate. Once this fluid is in the bleb, it will be absorbed by surrounding tissues, so it will not increase fluid pressure in your eye.
Invasive surgeries like trabeculectomy are reserved as a second line of treatment unless you have acute glaucoma threatening your vision. If eye drops or laser procedures do not work well enough to reduce the fluid pressure in your eye, your ophthalmologist will evaluate you to determine if trabeculectomy is the right procedure for your eye health.
Long-term studies show that, if needed, trabeculectomy is a fantastic treatment for glaucoma that often removes the need for prescription eye drops, which can be expensive. Although this is a more invasive operation, medical studies show that it is often more successful at keeping intraocular pressure low than both medication and laser operations.
In one study spanning 20 years, 90 percent of participants with trabeculectomy reported that their fluid pressure was still in a healthy range. Two-thirds did not need medication, while one-third still needed prescription eye drops to manage eye pressure.
Trabeculectomy Success Factors
The success of Trabeculectomy heavily depends on the surgery itself. However, frequent follow-ups for medications and scar/bleb management can improve success rates. Apart from anti-scarring drugs, your doctor may suggest alternative medications during your clinic visits.
For instance, depending on the progress of healing, your eye surgeon may decide to suture the trapdoor partially. The sutures will then be released occasionally during your visits to the clinic using a laser to allow more fluid to drain.
That said, about 10-12% of Trabeculectomy patients may require a repeat surgery. Studies also indicate that 20% of these procedures don’t control intraocular pressure for more than 12 months, and 2% fail every year after this time frame.
Patients with the highest failure risk include those with artificial lenses or whose bleb becomes encapsulated.
The Benefits of Necessary Trabeculectomy
The average cost of this operation without insurance coverage is about $7,872 per eye. Because of cost, health differences, and recovery time, you may receive trabeculectomy in only one eye at a time. This vision procedure is considered medically necessary, so your insurance should cover part or all of the cost.
Ultimately, the benefits outweigh the risks of glaucoma surgery. Your ophthalmologist will only recommend this step if they are concerned about high fluid pressure and vision loss, and they have already tried other methods of creating fluid equilibrium.
You deserve clear vision. We can help.
With 135+ locations and over 2.5 million procedures performed, our board-certified eye surgeons deliver results you can trust.
Your journey to better vision starts here.
References
- What Is Glaucoma? (August 2019). American Academy of Ophthalmology (AAO).
- Glaucoma Surgery. (October 2017). Glaucoma Research Foundation (GRF).
- Glaucoma Treatment. (August 2019). American Academy of Ophthalmology (AAO).
- Trabeculectomy. (2019). International Glaucoma Association (IGA).
- Incisional Surgery. (January 2017). Glaucoma Research Foundation (GRF).
- Glaucoma Surgery Series: The Risks and Benefits of Glaucoma Surgery. (April 2018). BrightFocus Foundation.
- Comparative Cost-effectiveness of the Baerveldt Implant, Trabeculectomy With Mitomycin, and Medical Treatment. (May 2015). Journal of the American Medical Association (JAMA), Ophthalmology.
- What is eye pressure? (September 2012). American Academy of Ophthalmology.
- Failure risks for Trabeculectomy. (December 2013). Journal of Current Glaucoma Practice.
- Minimally Invasive Glaucoma Surgery. (June 2013). Glaucoma Research Foundation.
This content is for informational purposes only. It may have been reviewed by a licensed physician, but is not intended to serve as a substitute for professional medical advice. Always consult your healthcare provider with any health concerns. For more, read our Privacy Policy and Editorial Policy.
