Uveitis: Causes, Symptoms, and How to Treat It Properly
Home / Eye Conditions & Eye Diseases /
Last Updated:
Uveitis is an uncommon eye condition marked by inflammation in the uvea, a part of your eye between the cornea and the retina. Uveitis has several different causes, including infections, immune reactions, injuries and even eye cancer.
Table of Contents
Uveitis can be treated, and it usually clears up in a few weeks with the appropriate medication. However, it is not safe to try to let the condition run its course without medical help.
Uveitis can lead to a range of serious complications, some of which can cause you to go permanently blind. You should a doctor as soon as possible if you experience any symptoms of uveitis.
What Is Uveitis?
Uveitis is an eye condition in which the uvea (part of the center of your eye) becomes inflamed. It can occur in all parts of the uvea. Each location is considered to be a different type of uveitis and has its own name. Some of the most common of these include:
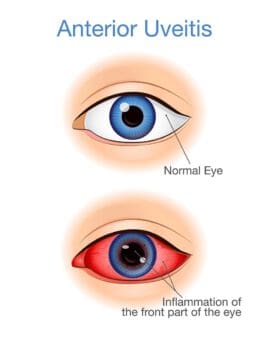
- Anterior uveitis, which affects the front part of the uvea
- Intermediate uveitis, which affects the vitreous humor (the clear structure in the center of the eye)
- Posterior uveitis, which affects the back part of the uvea
- Panuveitis or diffuse uveitis, which affects the entire eye
You deserve clear vision. We can help.
With 135+ locations and over 2.5 million procedures performed, our board-certified eye surgeons deliver results you can trust.
Your journey to better vision starts here.
Over time, uveitis may spread to other parts of your eye, including the:
- Lens
- Retina
- Cornea
- Sclera
- Vitreous humor
- Optic nerve
Without treatment, inflammation stemming from uveitis can lead to permanent tissue damage in any part of your eye where it is present. Your doctor might has several options to treat it using:
- Anti-inflammatory medication
- Antibiotics
- Immunosuppressant medication
- Surgery
What is the Uvea?
The uvea is the part of the eye that is located between the sclera (the visible white part of your eye) and the retina (the part of the eye that converts light into brain signals). It has three parts:
- The iris (the colored part of your eye)
- The ciliary body (the part of your eye that produces eye fluid)
- The choroid (a layer of blood vessels and connective tissue)
Types of Uveitis
While uveitis mainly affects the uvea, it can start or spread to other areas of the eye, eventually leading to blindness. There are several types of uveitis. The most often diagnosed versions include:
- Anterior uveitis: Also called iritis, this type of inflammation in the eye impacts the front parts of the uvea, especially the iris and the ciliary body. This is the most common form of uveitis in young and middle-aged adults. This condition is most often characterized by pain, light sensitivity, and blurry vision.
- Intermediate uveitis: Sometimes also called cyclitis, this form of the condition affects the vitreous humor, which is the clear gel-like structure in the center of the eye. It is also common in young adults. The most common symptoms of this type of uveitis include floaters and blurry vision.
- Posterior uveitis: Also called choroiditis or retinitis, this is the least common form of uveitis, and it primarily affects the back of the eye. Symptoms most common to posterior uveitis include decreased or lost vision along with floaters.
- Panuveitis: Also called diffuse uveitis, this form of inflammation harms the eye as a whole, not just the uvea.
- Drug-induced uveitis: Some prescription medications may cause inflammation, which increases the risk of uveitis. Topical formulas, periocular or intraocular injections, and medications that affect the whole body may trigger an inflammation response. If you have prescription medications and are concerned about this side effect, ask your doctor about the risk.
Aside from the areas of the eye that are inflamed, uveitis is also classified based on duration.
- Acute uveitis: This is short-term uveitis, which may last a few weeks or even a few months, but eventually clears up. While it may clear up on its own, it is best to be diagnosed by an eye doctor and get treatment to help acute uveitis clear up without damaging internal structures in the eye.
- Chronic uveitis: This lasts for several months to years, and it may recur frequently or never truly clear up.
Symptoms of Uveitis
If you have uveitis, you may notice symptoms such as:
- Blurry vision
- Floaters (dark spots that float across your field of vision)
- Photophobia (sensitivity to light)
- Eye pain
- Teary or watery eyes
- Eye redness
- Flashing effects in your vision
- Decreased vision
These symptoms usually appear suddenly and quickly get worse. However, they sometimes develop slowly over time.
Causes of Uveitis

There are four main causes of uveitis:
- Eye injury
- Eye surgery
- Viral infections like chicken pox, tuberculosis and herpes
- Inflammatory diseases like lupus, rheumatoid arthritis and AIDS
Rarely, uveitis may be a complication of eye cancer. Up to one third of uveitis cases also have no known cause.
You deserve clear vision. We can help.
With 135+ locations and over 2.5 million procedures performed, our board-certified eye surgeons deliver results you can trust.
Your journey to better vision starts here.
Risk Factors
There are certain risk factors that make you more likely to get non-infectious uveitis. These include:
- Vitamin D deficiency
- Autoimmune diseases
- Eclampsia and pre-eclampsia
- Taking certain medications, including immune checkpoint inhibitors, bisphosphonates or female hormone therapy
- Smoking
Uveitis is also more common in women and in anyone in the 20 to 50 age range.
When to See a Doctor
You should seek medical attention if you have persistent eye pain or any significant changes in vision. This is especially important if you have had a past case of uveitis.
Because uveitis is a very serious disease, many doctors are not comfortable treating it on their own. You may be referred to an ophthalmologist (an eye specialist) for diagnosis, treatment, or to determine what is causing your uveitis.
Diagnosis and Treatment of Uveitis

To receive a uveitis diagnosis, an optometrist or ophthalmologist will need to examine your eyes. You may also need to give a medical history, including any existing medical conditions and medications. If you have uveitis, it could indicate an underlying condition, so following a comprehensive eye exam with a visit to your general practitioner is wise.
An eye exam will include thorough examination of your eyes, along with:
- A visual acuity test, which may include the Snellen eye chart.
- A fundoscopic exam, in which the pupil is dilated, and a light is shone through with an ophthalmoscope, so your optometrist can examine the middle and back of your eye.
- Ocular pressure test involving a tonometer or a tonopen, which will touch the surface of your eye after you receive numbing drops and measure the internal pressure of your eye.
- A slit lamp exam, which uses a dye called fluorescein so the blood vessels throughout your eye can be seen more easily.
Your optometrist or ophthalmologist will try to avoid more invasive tests, but you may also need further medical exams or tests like:
- Blood tests.
- Fluid analysis from a sample of the vitreous humor.
- Angiography to examine the retinal blood flow.
- Photographic tests examining the thickness of retinal tissue to determine the presence or absence of fluid underneath the retina.
Based on the symptoms you experience, knowledge of any underlying conditions, and the results of tests, you may receive a uveitis diagnosis. If you have uveitis, your eye doctor will provide approaches to treatment that are primarily designed to reduce or eliminate inflammation. They also focus on alleviating pain, preventing tissue damage, and restoring as much lost vision as possible. The specific treatment you are prescribed will depend on what type of uveitis you have.
For example, anterior uveitis is treated with eye drops that dilate the pupil and prevent muscle spasms in the iris and ciliary body (called cycloplegics). You may also receive separate eye drops that contain a steroid like prednisone, which reduces inflammation, or you may receive a combined eye drop.
Intermediate, posterior, and panuveitis treatments may start with steroid eye drops, but they may also include injections in the eye, oral medications, or time-release capsules that are surgically implanted in the eye to manage chronic inflammation. If you are diagnosed with an autoimmune disease, you may take separate immunosuppressants that can alleviate some of your uveitis symptoms.
In some milder cases, you may take nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or acetaminophen to reduce inflammation and pain, or you may take these over-the-counter medicines in combination with other prescription treatments.
In more intense or chronic, recurrent cases, you may undergo surgery. Damage to the physical structures of the eye, including chronic diseases like cataracts or glaucoma triggered by uveitis, may require surgical procedures to restore vision. Another form of surgery you may need is a vitrectomy, which removes some of the vitreous gel from the middle of your eye, relieving pressure and removing some inflamed or infected tissue. Your ophthalmologist will let you know if or when this treatment is needed.
Complications of Uveitis
If uveitis is left untreated, it can lead to many serious complications. These include:
- Glaucoma, or damage to your optic nerve (the nerve that connect your eye to your brain)
- Cataracts, or clouding in the lens of the eye
- Cystoid macular oedema, or swelling of the retina
- Detached retina (when your retina pulls away from the blood vessels that support it)
- Posterior synechiae (when your iris sticks to the lens of your eye)
Several of these can lead to permanent blindness and other vision impairments. It is important to treat both uveitis and its complications as soon as you notice there is something wrong. The longer you wait, the higher the chance that you will experience irreversible damage.
FAQs About Uveitis
Yes, uveitis can cause blindness. Approximately 30,000 Americans go blind every year because of untreated uveitis.
What does uveitis pain feel like?
Pain from uveitis feels like a dull ache in and around your eye. This pain may become sharper when your gaze is focused on something.
Can uveitis be cured?
There is no permanent cure for uveitis. Treatment will help an ongoing case of uveitis to clear up, but once you have it, it is always possible that it will come back. Some people only suffer one attack of uveitis in their lives, while others experience multiple flare-ups over the years.
Can uveitis go away on its own?
In some mild cases, uveitis will abate without treatment. However, this is not usually the case And untreated uveitis can have severe consequences like blindness.
Is uveitis the same as pinkeye?
Uveitis may look like pinkeye to a non-professional, but it is very different. If you have pinkeye that has not responded to typical treatments, it may be a good idea to have it checked again to be sure it isn’t actually uveitis.
Is uveitis contagious?
No, but the viruses that sometimes cause it are. If you have uveitis and don’t know why, it’s best to act as if you are contagious and avoid direct contact with others for the time being.
You deserve clear vision. We can help.
With 135+ locations and over 2.5 million procedures performed, our board-certified eye surgeons deliver results you can trust.
Your journey to better vision starts here.
References
- Facts About Uveitis. (August 2011). National Eye Institute (NEI), National Institutes of Health (NIH).
- Uveitis: A Guide to Your Condition and Its Treatment. (December 2016). AbbVie.
- Uveitis: Overview. (June 5, 2018). Mayo Clinic.
- What Is Uveitis? (August 22, 2018). American Academy of Ophthalmology (AAO).
- Drug-Induced Uveitis. (March 13, 2013). Journal of Ophthalmic Inflammation and Infection.
- Uveitis Causes. (August 22, 2018). American Academy of Ophthalmology (AAO).
- Uveitis: What You Need to Know. (March 7, 2017). Medical News Today.
- Uveitis: Diagnosis. (June 5, 2018). Mayo Clinic.
This content is for informational purposes only. It may have been reviewed by a licensed physician, but is not intended to serve as a substitute for professional medical advice. Always consult your healthcare provider with any health concerns. For more, read our Privacy Policy and Editorial Policy.
