Drugs and Macular Degeneration: What Drugs Cause It?
Last Updated:
Table of Contents
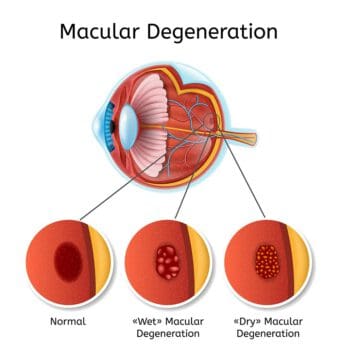
Macular degeneration is the loss of central vision due to degeneration or damage to the macular, a smaller part of the retina. This condition is associated with age, but some drugs may increase your risk of AMD.
There are two basic types of macular degeneration, both of which are closely associated with genetics and family history. However, there are some lifestyle factors like diet and smoking that increase the risk of this vision damage.
Smoking is associated with damage to blood vessels, reduced oxygen flow, fewer nutrients circulating in the body, and higher rates of harmful chemicals in the body, which can all lead to damage to the retina and, specifically, the macula.
High blood pressure can increase your risk of AMD. Blood pressure medications have also been associated with a higher risk of macular degeneration.
Discuss your risks of AMD with your doctor and ophthalmologist. If you are diagnosed with this condition, certain lifestyle changes and some medical treatments can slow the progression of vision loss.
Macular Degeneration: Can Drugs Cause This Type of Vision Loss?
Macular degeneration is a common vision problem involving damage to the retina.
The macula is the area on the retina that sends central vision images to the brain. When this area is damaged or degenerates, your central vision becomes blurry or darker. Eventually, it goes away completely. You will probably retain peripheral vision as this occurs, but peripheral vision is less focused than your central vision.
You deserve clear vision. We can help.
With 135+ locations and over 2.5 million procedures performed, our board-certified eye surgeons deliver results you can trust.
Your journey to better vision starts here.
Age-related macular degeneration (AMD) is the most common cause of blindness in adults, aged 50 and older, in the United States. AMD is more common than cataracts and glaucoma. It is rare for children or young adults to develop macular degeneration, but Stargardt macular degeneration is an inherited condition that affects about 1 in every 8,000 to 10,000 individuals.
While AMD is most closely associated with genetics and age, there are some external factors that increase the risk of developing macular degeneration or trigger the condition earlier in life. These include using blood pressure medications in the vasodilator family and smoking cigarettes.
Types of Macular Degeneration and AMD Risk Factors
There are two types of macular degeneration.
- Dry AMD: This is the most common version of AMD, affecting 80 percent of people ages 50 and older who develop macular degeneration. Dry AMD may develop in one eye first, but the condition will eventually impact both eyes. Drusen, yellow deposits that build up under the retina, accumulate in people who have dry macular degeneration. While they are not considered the cause, they are closely associated with the condition. Symptoms of dry AMD include:
- Visual distortions, like straight lines appearing bent.
- Reduced central vision.
- Needing brighter light when reading or performing other close tasks.
- Increasing trouble adapting to low light levels, like entering a dimly lit restaurant.
- Increased blurriness of printed words.
- Decreased brightness or intensity of colors.
- Trouble recognizing faces.
- Wet AMD: This type of macular degeneration begins as dry AMD but progresses faster, leading to rapid vision loss when blood vessels form under the retina and leak blood onto the macula. Symptoms of wet macular degeneration include:
- Visual distortions.
- Reduced central vision in one or both eyes.
- Decreased intensity of colors.
- Blurry spot formation in the center of your vision, often in a well-defined area.
- General haziness in your vision overall.
- Abrupt onset of these symptoms.
Neither type of macular degeneration has a specific cause, and they are both associated more with age-related conditions and genetic predisposition than any other specific cause. There are some risk factors that increase your chances of developing AMD, which you can control, including:
- Eating foods that are high in fat and cholesterol, and that have a high glycemic index, like processed meats, cheese, or starches.
- Not eating enough fruits and vegetables, or otherwise experiencing vitamin deficiency.
- Having a high body mass index (BMI) at 30 or higher.
- Having high blood pressure, which restricts oxygen to various parts of the body, including the retina.
- Having a sedentary lifestyle.
- Smoking.
Smoking: A Controllable Risk Factor Associated With Macular Degeneration

Several medical studies have shown that smoking exacerbates your risk of eye disease, especially macular degeneration. People who smoke a pack a day or more reportedly double their risk of blindness when they reach elderly adulthood. The more frequently you smoke and the longer you smoke throughout your life, the higher your risk of macular degeneration.
Smoking likely speeds up deterioration of the macula because chemicals in cigarettes reduce the number of protective nutrients delivered through the bloodstream to the eye and increase the number of damaging chemical compounds deposited in that area. Smoking also reduces oxygen flow to the eye by constricting blood vessels, similar to the effects of high blood pressure.
The University of Manchester researchers found that smokers are four times more likely than nonsmokers to develop AMD. However, former smokers have only a slightly higher risk of developing AMD compared to those who never smoked, suggesting that the damaging effects of smoking on the eye can be reversed if you quit.
You deserve clear vision. We can help.
With 135+ locations and over 2.5 million procedures performed, our board-certified eye surgeons deliver results you can trust.
Your journey to better vision starts here.
Blood Pressure Drugs and a Higher Risk of Macular Degeneration
Data on the correlation between high blood pressure and AMD has been inconsistent over the years, but there is some relationship between the two conditions. However, some medical research has also shown a connection between taking vasodilators to lower blood pressure and a higher risk of AMD.
A long-term study at the University of Wisconsin School of Medicine, spanning 1988 to 2013, found that taking any vasodilator increased the risk of early-stage AMD. The study examined the eye health of 5,000 participants during several decades. Among those not taking vasodilators like Apresoline and Loniten, about 8.2 percent developed signs of early age-related macular degeneration. Among those taking vasodilators, about 19.1 percent developed the disease.
The research team also found that oral beta blockers like Tenormin and Lopressor increased the risk of neovascular or wet AMD. In the population not taking beta blockers, about 0.5 percent developed wet AMD. In the population taking beta blockers, about 1.2 percent developed this more serious form of macular degeneration.
If your doctor prescribes a medication to lower your blood pressure, it is likely that you have a chronic condition that requires management to improve your quality of life. Discuss the risks associated with this prescription with your doctor, especially if you have a family history of age-related macular degeneration or have already developed this condition.
Treating Macular Degeneration
Smoking is a risk factor for AMD that is within your control. Work with your physician to quit smoking. They can prescribe medications that can help.
There are other factors like diet and exercise that may impact your blood pressure too. If you have high blood pressure, your doctor may recommend lifestyle changes to lower it.
If your doctor prescribes blood pressure medication, this lifesaving treatment is not exactly within your control. Concerns about your eye health should be brought up with your prescribing physician and your optometrist or ophthalmologist, especially if you have a higher risk of AMD due to genetics and family history. These factors are not in your control, but you can manage your risk of AMD or work with a specialist to slow the progression of macular degeneration if you develop the condition.
There is no direct treatment for dry AMD, but your doctor may recommend taking vitamins and minerals to slow the progression. Good options include the following:
- Vitamin C
- Vitamin E
- Lutein
- Zeaxanthin
- Zinc
- Copper
Wet AMD can benefit from treatment with anti-VEGF drugs. These treatments reduce the number of abnormal blood vessels forming around and under your retina, which can slow the degeneration of the macula. Laser surgery is also becoming an increasingly common approach to reducing blood vessels that can damage your macula.
Your eye doctor will monitor the changes in your eye and work with you to manage symptoms as much as possible. This also includes understanding how to make the most of low vision and peripheral vision. Magnifying tools, special computer settings or programs, and other tools can help you continue to participate in activities as long as possible. You can also work with a vision rehabilitation specialist for low vision support.
You deserve clear vision. We can help.
With 135+ locations and over 2.5 million procedures performed, our board-certified eye surgeons deliver results you can trust.
Your journey to better vision starts here.
References
- What Is Macular Degeneration? (May 2019). American Academy of Ophthalmology (AAO.org).
- Stargardt Macular Degeneration. (November 2019). Genetics Home Reference, National Institutes of Health (NIH).
- Dry Macular Degeneration. Mayo Clinic.
- Wet Macular Degeneration. (August 2019). Mayo Clinic.
- Macular Degeneration: Prevention & Risk Factors. BrightFocus Foundation.
- Don’t Smoke – It Exacerbates Eye Disease. American Macular Degeneration Foundation (AMDF).
- Research News: Blood Pressure Drugs and AMD. (May 2014). American Academy of Ophthalmology (AAO).
- How Is AMD Diagnosed and Treated? (May 10, 2019). American Academy of Ophthalmology (AAO.org).
- Macular Degeneration and Low Vision: Making the Most of Low Vision. (May 10, 2019). American Academy of Ophthalmology (AAO).
This content is for informational purposes only. It may have been reviewed by a licensed physician, but is not intended to serve as a substitute for professional medical advice. Always consult your healthcare provider with any health concerns. For more, read our Privacy Policy and Editorial Policy.
