Signs of Ocular Herpes and Treatment Options
Home / Eye Conditions & Eye Diseases /
Last Updated:
Table of Contents
Ocular herpes, also referred to as eye herpes, is a condition often mistaken for regular pink eye. If you have long-lasting or especially severe keratitis (inflammation of the cornea), it could be a sign your condition is more serious than it first appeared.
Ocular herpes is first contracted through either the herpes simplex virus or herpes zoster, commonly called shingles.
Usually a person is first infected with the virus HSV-1 in their youth, and the virus can end up infecting the eye. This initial infection can go unnoticed, showing few symptoms (if any) or symptoms that are similar to pink eye.
Even if it seems to go away, it may lay dormant in the eye, causing future problems. This can alternatively happen with shingles, through a similar process, but generally later in life.
When the latent herpes reactivates, either randomly or through triggers that are difficult to determine, it can cause serious eye problems, including epithelial keratitis, stromal disease, and endotheliitis. While some of these diseases are more serious than others, all can cause blindness and other vision problems if left untreated.
Even if eye herpes itself has no cure, it can be treated with medications, as can the diseases it causes. This is usually done with some mix of antivirals and steroids, depending on what your doctor deems appropriate.
There is not always an easy lab test to confirm ocular herpes, and it can be mistaken for a few conditions. If your doctor has been unable to diagnose your condition, or diagnosed you and your prescribed treatment is not working as it should, consider seeing a specialist to check if you were misdiagnosed or if there are other treatments available.
Ocular Herpes, HSV, and Shingles

When active, the virus can cause complications in the eye. Talk to a doctor as soon as possible if you have herpes simplex virus (HSV) or herpes zoster (shingles) and notice any eye-related issues. Speedy treatment can help to prevent serious damage and mitigate future risks.
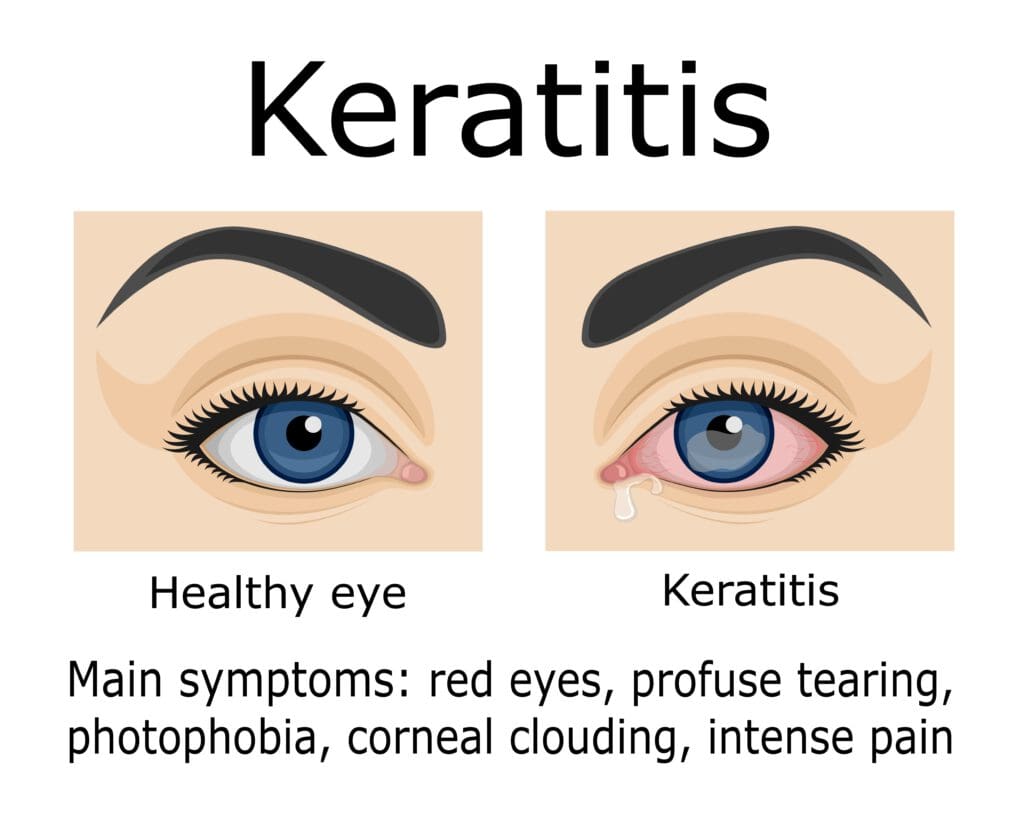
One potential sign of ocular herpes is keratitis, an inflammation of the cornea. Herpes is not the only thing that can cause keratitis, but you should still see a doctor to determine how serious your condition is because of how serious any eye complication can be.
You deserve clear vision. We can help.
With 135+ locations and over 2.5 million procedures performed, our board-certified eye surgeons deliver results you can trust.
Your journey to better vision starts here.
What Causes HSV/Shingles?
HSV-1 is transmitted via oral fluids, while HSV-2 is transmitted via the genitals. It is HSV-1 that is commonly associated with eye herpes.
While some associate herpes specifically with sexual contact, this is not necessarily how one gets the infection. HSV-1 can infect the genitals through oral sex, however.
Both conditions are chronic, although they can be managed with treatment.
Many people with HSV may be asymptomatic or mildly asymptomatic to the point that they do not notice their condition, spreading it accidentally. An estimated 67 percent of the world’s population has some form of HSV. It should be noted that this does not mean 67 percent of the world’s population has ocular herpes, which is much rarer.
HSV is usually first caught in youth, where symptoms may be mild or go unrecognized.
In the case of ocular HSV, this primary infection enters the eye and eventually reaches the trigeminal ganglion, going latent. It will remain there for life, occasionally traveling back to the cornea, which in turn causes chronic problems with eye disease through recurrent infections.
Shingles gets into the eye more rarely but with a similar effect. It is a serious condition in its own right, characterized by painful rashes caused by the same virus that causes chickenpox. If you have ever had chickenpox, you might develop shingles, although not everyone does. Additionally, even fewer people will have herpes zoster/shingles infect their eye.
Exactly what causes the recurrent infections that characterize ocular herpes is not entirely clear. Some proven triggers include the following:
- UV light
- Fever
- Refractive surgery
- Cold
- Periods
- Illness or high fever
- Otherwise weakened immune system
Some people seem to be triggered randomly, and other patients anecdotally report a wide variety of triggers beyond the above list.
Stress is one commonly reported trigger, but the Herpetic Eye Disease Study (HEDS) group says it does not actually seem to be a trigger of HSV recurrent infections. They do additionally admit that stress is a difficult trigger to totally disprove, as it has such a wide variety of meanings from patient to patient.
Common Confusions
There is no definitive test for the conditions sometimes caused by eye herpes, with the exception of HSV epithelial disease (discussed later). Some conditions ocular herpes might be misdiagnosed as include:
- Acanthamoeba infection.
- Topical medication toxicity.
- Healing abrasions.
According to Dr. James Chodosh, a doctor diagnosing diseases caused by ocular herpes might also find some difficulties over the lack of a simplified, widely accepted set of terminology. This can lead some doctors to improperly classify a given patient’s condition.
Is It Pink Eye or Ocular Herpes?
It’s common to mistake primary HSV infections for conjunctivitis. Ocular herpes often presents with the same symptoms as conjunctivitis, leading some physicians to assume it’s just garden-variety “pink-eye.”
Pink eye is significantly more common, affecting about 3 million people annually in the United States. In comparison, about 50,000 new and recurring cases of ocular herpes are diagnosed each year.
Even though the two conditions present somewhat similarly, there is a critical distinction between the two. Ocular herpes is the most common cause of infectious corneal blindness in the Western world.
Your doctor can make the correct diagnosis by conducting a culture test. If you have ocular herpes, the culture will test positive for type 1 or type 2 HSV.
Fortunately, both mild and severe ocular HSV infections can be treated with antiviral medication. But it’s imperative to correctly diagnose the condition and treat it early to prevent severe damage to the cornea.
You deserve clear vision. We can help.
With 135+ locations and over 2.5 million procedures performed, our board-certified eye surgeons deliver results you can trust.
Your journey to better vision starts here.
Epithelial Keratitis, Stromal Disease, and Endotheliitis
While ocular herpes can cause a variety of eye complications, the most serious is keratitis. There are essentially two types of keratitis: epithelial disease and stromal disease
Epithelial keratitis can cause redness, photophobia, tearing, blurred vision, and more in an infected eye. It is one of the most common manifestations of HSV keratitis and can cause serious vision problems and even blindness if left untreated.
Stromal keratitis (stromal disease) is very serious and can cause permanent blindness due to corneal scarring and astigmatism. There is also endotheliitis, a rare complication of ocular herpes, caused by endothelial problems in the eye. Like all of these complications, it can cause permanent damage left untreated. It is characterized by corneal edema, deposits on the corneal endothelium, mild eye pain, blurred vision, sensitivity to light, a small pupil, and redness.
Treatment
If your doctor determines you have ocular herpes, they will immediately prescribe antiviral medication. No cure yet exists for herpetic eye disease. The antiviral medications available today only suppress the reproduction of the virus; they do not eradicate the virus in its dormant state.
Treatment options for ocular herpes differ somewhat depending on the severity of the infection.
Epithelial Keratitis Treatment
Epithelial keratitis is a milder form of ocular herpes and usually affects the surface layer of the cornea. It can subside on its own, but antiviral medication can help minimize cornea damage.
Your doctor might prescribe an antiviral eye drop or oral antiviral medication like acyclovir (Zorivax).
They might also prescribe a topical ointment you can apply gently on the eyelids. While antibiotic ointments do not treat herpes infections, they will prevent a bacterial infection that might further damage the eyes.
Stromal Keratitis Treatment
Stromal keratitis is a more severe form of ocular herpes that affects the deeper middle layers of the cornea. Your doctor might prescribe antiviral eye drops or oral antiviral medications to help fight off the virus.
Since stromal keratitis is also associated with significant inflammation of the eye, your doctor might prescribe an anti-inflammatory medication such as steroids.
In some cases, the patient might never be able to come off steroids once they start treatment. Stromal keratitis can be chronic, and this might require several rounds of steroids treatment. That said, with endotheliitis, patients will be able to come off steroids.
Your doctor will work with you to determine the least possible dose of steroids you need. They can do this by gradually tapering your dose to find the specific dose needed to avoid the adverse side effects of steroids.
Intraocular pressure (eye pressure) can rise due to inflammation. If so, your doctor might also prescribe a pressure-lowering medication.
Recovering from eye herpes
It’s imperative to take medication as prescribed by your doctor. You should see improvement in two to five days. And the symptoms should dissipate within two to three weeks.
You deserve clear vision. We can help.
With 135+ locations and over 2.5 million procedures performed, our board-certified eye surgeons deliver results you can trust.
Your journey to better vision starts here.
References
- Demystifying the Ocular Herpes Simplex Virus. (January 2013). American Academy of Ophthalmology.
- Herpes Simplex Eye Infections. (October 13, 2016). UK NHS.
- Herpes Simplex Virus. (January 31, 2017). World Health Organization.
- Keratitis. (November 8, 2018). Mayo Foundation for Medical Education and Research (MFMER).
- Shingles. (May 16, 2018). Mayo Foundation for Medical Education and Research (MFMER).
- The Three Faces of Herpes Simplex Epithelial Keratitis: A Steroid-Induced Situation. (April 2, 2015). BMJ Case Reports.
- Herpes Simplex Virus Keratitis: A Treatment Guideline – 2014 (July 2014). American Academy of Ophthalmology.
- Herpetic Epithelial Keratitis. (December 18, 2014). QJM: An International Journal of Medicine.
- Treatment and Management of Presumed Herpes Simplex Keratouveitis With Endotheliitis. (2017). American Academy of Optometry.
- Keratic Precipitates. Columbia University Department of Ophthalmology.
- HSV Keratitis: An Important Infectious Cause of Blindness. (April 16, 2015). U.S. Pharmacist.
- Herpes Simplex Virus Keratitis: A Treatment Guideline – 2014. (June 2014). American Academy of Ophthalmology.
This content is for informational purposes only. It may have been reviewed by a licensed physician, but is not intended to serve as a substitute for professional medical advice. Always consult your healthcare provider with any health concerns. For more, read our Privacy Policy and Editorial Policy.
