The Causes of High Eye Pressure (& How to Treat Them)
Home / Eye Conditions & Eye Diseases /
Last Updated:
High eye pressure occurs when your eye has enough input of aqueous humor but cannot drain it properly through the trabecular meshwork.
Table of Contents
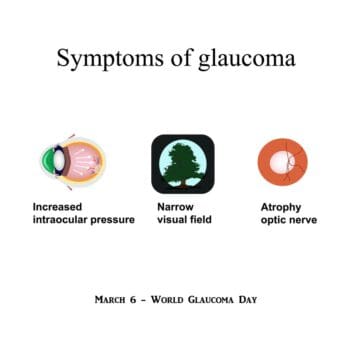
With routine eye exams, your optometrist or ophthalmologist can pressure test your eyes and monitor you for signs that your vision might be worsening. The biggest risk for untreated elevated intraocular pressure is glaucoma, which can lead to significant vision loss or blindness.
Medicated eye drops and a few surgical options are currently the best methods for treating glaucoma. Ultimately, you do not need treatment just for ocular hypertension, but monitoring the condition before it turns into glaucoma is important for your long-term vision health.
Research regarding high eye pressure is ongoing, and new studies continue to shed insight on its causes, risk factors, and potential treatments.

High Eye Pressure: What Does It Mean?
The trabecular meshwork is the spongy tissue near the cornea and iris that keeps the flow of your eye’s aqueous humor going. The aqueous humor keeps your eye’s shape, keeps nutrition flowing to vital structures, and eliminates waste through the trabecular meshwork. About 80 to 90 percent of the aqueous humor makes its way into and out of circulation because of this drainage system.
In healthy eyes, the meshwork keeps a fluid balance; however, this area can become clogged or stopped up for a range of reasons, causing the inflow of aqueous humor to be higher than the outflow. This causes high fluid pressure in the eye, which is risky. High fluid pressure can lead to problems with your vision, ranging from trouble seeing in the dark to retinal detachment.
You deserve clear vision. We can help.
With 135+ locations and over 2.5 million procedures performed, our board-certified eye surgeons deliver results you can trust.
Your journey to better vision starts here.
Glaucoma is nearly always associated with high intraocular pressure (IOP) or high fluid pressure in the eye. However, not every instance of high IOP leads to glaucoma. Ocular hypertension may just require monitoring to ensure there is no damage, without moving to prescription or surgical treatments.
How Do You Know If You Have High Eye Pressure?
Routine eye exams often look at your IOP. You may have sat through an examination in which a puff of air hit your eye. This device used to be the standard for optometrists and ophthalmologists to measure your eye’s fluid pressure, but a newer, more accurate device may be used instead.
This is tonometry, which involves a pen-like device with a circle of blue light on the end. Your doctor will numb your eyes with eye drops, and then press the device to your eye and directly measure the pressure. Tonometry allows for very accurate readings of pressure, so if you have slightly elevated pressure but no other changes, your eye doctor will know to follow up at your next exam.
Normal eye pressure ranges from 12 to 22 millimeters of mercury (mm Hg). If your eye pressure is more than 22 mm Hg, your doctor may examine your eyes more extensively for potential signs of damage. When your eyes are otherwise normal but your IOP is elevated, this is considered ocular hypertension.
Potential causes of ocular hypertension include:
- Age.
- Genetics
- Certain diseases, including cardiac hypertension or diabetes.
- High myopia (nearsightedness).
- Some medications for other conditions.

If you do have high fluid pressure, your doctor will also examine your eyes for:
- Visual acuity measurements to see if you have experienced blurring or double vision.
- Pachymetry, which measures corneal thickness.
- Visual field testing, which determines if you have spots of low vision or vision loss, especially in your peripheral vision.
- Evaluation of your retina to see if there is any damage to this or to your optic nerve.
- Gonioscopy, which helps your eye doctor see the angle of closure around the trabecular meshwork.
Someone who has high IOP is considered a glaucoma suspect. This is due to concern that glaucoma will develop, which is the beginning of vision loss.
Does High Eye Pressure Always Require Treatment?
Many people with high IOP do not need treatment. Regular monitoring ensures that your eyes are healthy and vision issues are addressed.
A 2021 study in JAMA Ophthalmology revealed that high eye pressure does not necessarily require treatment. Among study participants, those who delayed treatment did not experience significantly different outcomes than those who did not.
Another long-term study examining almost 3,300 subjects with elevated IOP, all between the ages of 40 and 80, looked at treating high eye pressure before glaucoma versus waiting. Researchers found that, over decades, there was not much difference between the patients who received treatment immediately and those who did not. The study concluded that monitoring eye pressure meant intervention came sooner, and more people kept their sight.
Ultimately, the best treatment approach and timeline will depend on a variety of personal factors. Discuss these with your doctor to best determine how to proceed.
You deserve clear vision. We can help.
With 135+ locations and over 2.5 million procedures performed, our board-certified eye surgeons deliver results you can trust.
Your journey to better vision starts here.
Dangers: Glaucoma
One type of glaucoma, normal tension or low tension glaucoma, involves damage to the retina without high intraocular pressure as a warning sign. However, other types of glaucoma involve high IOP as the first symptom and then progressive vision loss, especially if the condition is untreated.
Some types of glaucoma include:
- Primary open-angle glaucoma, which is the most common form. Vision loss, as progressive tunnel vision, occurs over several years.
- Angle-closure glaucoma, which causes vision loss on the day it begins. It is considered a medical emergency.
Glaucoma is often inherited. If your family has a history of it, you are at higher risk for developing it. Talk to your optometrist about your family’s history of glaucoma during your routine eye exam, so your doctor can keep track of your IOP and catch glaucoma early. This will help them develop a less invasive treatment plan and best preserve your vision.
Per a 2021 study, high levels of caffeine consumption can triple the risk of glaucoma for those who are already predisposed to high eye pressure. If you have a family history of high eye pressure and glaucoma, it may be wise to limit caffeine intake.
Treating Glaucoma
Your doctor will create a specific treatment plan for your glaucoma, which may include medication or surgery. New approaches to treating glaucoma are in development. In the meantime, the most common courses of treatment are:
- Medicated eye drops. There are several types of prescription eye drops that can treat glaucoma. Your eye doctor may prescribe one and see how well it works, or they may prescribe a combination of several and check in on you later. If eye drops alone work, you can maintain this course of treatment for years with little further vision loss.
- Laser surgery. As more eye surgeons use laser devices to treat vision problems with outpatient operations, there are more options that are less invasive for patients, which allows for faster healing and greater satisfaction. There are two types of laser surgery for glaucoma treatment.
- Trabeculoplasty: This is specifically for those with open-angle glaucoma. A laser forces the drainage system to open and allow more fluid to flow through.
- Iridotomy: This surgery treats angle-closure glaucoma, which is a medical emergency. A laser creates a hole in the iris, forcing fluid out through a new drainage channel.
- Operating room surgery. General anesthesia and long healing times make operating room surgeries the last resort, but your eye doctor may still recommend a surgical procedure if your glaucoma resists other forms of treatment. Like laser surgery, there are two types of operating room surgery.
- Trabeculectomy: Your surgeon creates a tiny flap in the sclera and then creates a bubble in your conjunctiva, which is called a bleb. The bleb collects aqueous fluid and distributes it across the conjunctiva or sclera, where it is reabsorbed by other tissues, but taken out of circulation so it does not impact eye pressure.
- Glaucoma drainage devices: In some situations, your doctor may need to implant a drainage tube into your eye. This sends fluid to a collection area called a reservoir, which is under the conjunctiva. Aqueous humor is then absorbed into blood vessels that are nearby.

High Fluid Pressure Should Be Monitored Before It Turns Into Glaucoma
Getting regular eye exams is vital to your eyes’ long-term health. Without these exams, you may develop a condition like ocular hypertension or glaucoma and not realize you are losing your sight until you are struggling.
With eye pressure tests, your optometrist or ophthalmologist can monitor your eyes for elevated pressure and then check for potential vision loss. When you begin to lose your sight, just as glaucoma begins, your doctor can create a treatment plan that will slow the progress of this condition.
Overall, regular eye exams are the best way to preserve your vision if you have glaucoma. Early diagnosis and intervention, when needed, ensure that the progression of the condition can be slowed, and your vision can be managed.
You deserve clear vision. We can help.
With 135+ locations and over 2.5 million procedures performed, our board-certified eye surgeons deliver results you can trust.
Your journey to better vision starts here.
References
- Glaucoma and the Importance of the Eye’s Drainage System. (February 2017). BrightFocus Foundation.
- Eye Pressure Testing. (February 2018). American Academy of Ophthalmology (AAO).
- High Eye Pressure and Glaucoma. (October 2017). Glaucoma Research Foundation.
- Ocular Hypertension. Bausch + Lomb.
- Glaucoma. American Optometric Association (AOA).
- Glaucoma Treatment. (February 2020). American Academy of Ophthalmology (AAO).
- High Eye Pressure: Monitor or Treat? (March 2010). The Source, Washington University in St. Louis.
- High Caffeine Consumption May Be Associated With Increased Risk of Blinding Eye Disease. (June 2021). Mount Sanai.
- High IOP May Not Necessarily Require Treatment, Results From New Study Suggests. (May 2021). Optometry Times.
- Effectiveness of Elevated Intraocular Pressure as a Criterion for Glaucoma Referral After 6 Years of Follow-Up. (April 2021). Dovepress.
This content is for informational purposes only. It may have been reviewed by a licensed physician, but is not intended to serve as a substitute for professional medical advice. Always consult your healthcare provider with any health concerns. For more, read our Privacy Policy and Editorial Policy.
