
Medically Reviewed by John Davidson, M.D. NVISION Surgeon
Your Guide to Cataracts: Signs, Stages, Effects & More
Home /
Last Updated:

Medically Reviewed by John Davidson, M.D. NVISION Surgeon
Table of Contents
What Are Cataracts?
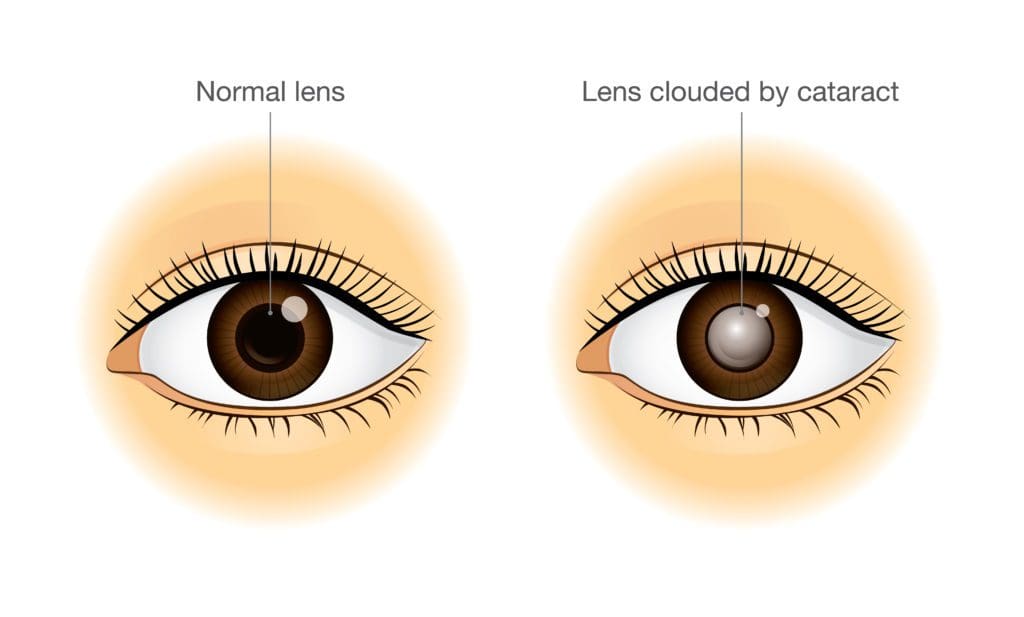
The National Eye Institute (NEI) defines cataracts as clouding in the lens of the eye. When your lens is clouded, your eye struggles to focus light on your retina. The result is hazy, blurry, or less vibrant vision.
Common cataract symptoms include the following:
Don't Let Cataracts Limit Your Life
With 135+ locations and over 2.5 million procedures performed, our board-certified cataract surgeons have the experience you can trust. Take the first step toward seeing clearly again.
Restore Clarity to your World Today.
- Blurred vision
- Double vision
- Light sensitivity
- Halos or similar effects around lights
- Poor night vision
- Colors appearing faded
- Frequent prescription changes for glasses and contacts
- Dizziness
The earliest major problems many people encounter are difficulty reading and driving.
Untreated cataracts tend to progress until they impact a person’s quality of life. Eventually, seeing out of an affected eye may be difficult or impossible.
Key Facts About Cataracts
- Cataracts are more common in women than men, with a male-to-female ratio of about 1 to 1.3.
- Of older people with cataracts in both eyes, almost 86 percent struggle with nighttime driving, and about 74 percent have difficulty driving in the rain.
- Cataracts are so common in older people that some consider them a natural part of the aging process.
- Cataracts are among the leading causes of blindness in the United States. Unlike other blinding conditions (like glaucoma), cataracts can be treated quickly and effectively with a laser-based surgical procedure.
What Are the Different Types of Cataracts?
All cataracts involve clouding in the part of your eye that focuses light, but the reasons for that clouding can vary.
The NEI recognizes five main types of cataracts.
Age-Related Cataracts
Cataracts are a common eye condition among aging adults, with over 50 percent of people over 80 developing them. Cataracts are more common among older adults who smoke, drink excessive amounts of alcohol, or use steroid medications.
Traumatic Cataracts
Every day, about 2,000 American workers sustain an eye injury that requires medical care. Some of these injuries can cause cataracts. An injured eye must heal, and during that process, rogue cells can clump together and cause lens clouding.
Radiation Cataracts
The sun’s rays do more than darken skin. Some types of sunlight can harm tissues deep inside the eye, sparking changes that can lead to cataracts. UV-based radiation treatments for some types of cancer can also cause cataracts.
Congenital Cataracts
Some babies are born with genetic defects that can lead to cataracts. This form of cataract is relatively rare, but the problem tends to run in families. Treatment early in life can help a baby to see better.
Secondary Cataracts
Also known as posterior capsule opacification, secondary cataracts arise due to scar tissue formation after cataract surgery. Up to 2 in 5 people who have cataract surgery will develop this complication. A quick surgical procedure fixes it.
What Causes Cataracts?
The most common cause of cataracts is aging, as proteins in the eye break down as part of the natural aging process. These proteins can form clumps, which can get bigger over time and affect vision.
Other forms of cataracts appear as eye tissues heal from drug exposure, UV radiation, or surgery. And some cataracts arise due to congenital issues no one can predict or control.

Don't Let Cataracts Limit Your Life
With 135+ locations and over 2.5 million procedures performed, our board-certified cataract surgeons have the experience you can trust. Take the first step toward seeing clearly again.
Restore Clarity to your World Today.
How Do Doctors Check for Cataracts?
To diagnose cataracts, a doctor will dilate your eye, widening your pupil and making it easier to look for cataracts.
Cataracts are diagnosed with a visual exam, and if they’re found, your doctor can measure them and mark their size and location in your chart. You could be referred for treatment right away based on the size, or your doctor could ask you to come back for recheck appointments to measure its progress.
This diagnosis process is usually painless, although dilation can be uncomfortable, and it takes a few hours to wear off. You will usually need someone to drive you home, as your eye will be especially sensitive to light when artificially dilated.
How Are Cataracts Treated?
Once you and your doctor decide your cataracts affect your life enough to justify surgery, your doctor has several surgical options available.
Cataract surgery is very safe and effective, allowing most people to return to a similar quality of life as they had before cataracts began to affect their vision.
Phacoemulsification
Phacoemulsification is the most common type of cataract surgery. It involves making a small incision and breaking the eye’s natural lens into pieces. These pieces are then sucked out of the eye, and an intraocular lens (IOL) is inserted in its place. This synthetic lens helps focus light onto your retina, much like your natural lens would.
Extracapsular Surgery
Extracapsular surgery involves a larger incision compared to phacoemulsification. The harder, central part of your lens is removed, and the remaining pieces are removed. Next, an IOL replaces your removed lens.

Cataract Surgery
Cataract eye surgery is a very common and medically necessary procedure to remove and replace the eye’s natural lens when the vision has been clouded by a cataract. We offer laser-assisted cataract surgery and lifestyle lenses as options for our patients.
Emerging Research on Cataracts
While experts agree that cataracts are a common part of the aging process, they’re not sure why these problems develop. In February 2022, the NEI offered a $1.6 million grant to a team with the University of Arizona College of Medicine studying the biological mechanisms behind cataracts.
Research like this could help future doctors treat emerging cataracts more effectively. The research might also help doctors develop tools to delay the onset of cataracts in their older patients.
Researchers are also performing studies to examine surgical techniques. A traditional cataract removal procedure involves specialized equipment, including suction devices. Some researchers believe using lasers is more effective and results in better results for patients.
Cataract Frequently Asked Questions
Is there a cure for cataracts?
Cataracts cannot be cured, but surgery can remove an affected lens and insert a synthetic lens that allows a person’s clear vision to return. Cataract surgery is essentially a “cure” for the issue since the cataract is removed.
There is no way to get rid of a cataract after it has formed other than surgery. The cataract must be removed to repair vision in that eye.
Can eye drops dissolve cataracts?
While some unscrupulous companies claim otherwise, it is impossible to “dissolve” a cataract. No at-home treatment exists that can fix cataracts. The only solution currently available is to remove the affected lens and put a synthetic lens in its place.
Can cataracts go away on their own?
No, the only treatment for cataracts is surgery to remove the natural lens and put in a synthetic lens.
Can cataracts come back after surgery?
No. Since the natural lens is replaced with a synthetic lens, cataracts cannot return after surgery. A cataract cannot develop on an artificial lens.
Can cataracts cause headaches?
If they’re left untreated, cataracts can make it hard for you to see clearly. Some people develop eye strain if they try to drive at night or read in low-light conditions. But headaches aren’t common in people with small, early-stage cataracts.
Can cataracts be reversed?
Only surgery can fix cataracts. You can use sunglasses, eat nutritious food, and quit smoking to stop them from growing quickly, but cataracts can’t be reversed.
What are cataracts made of?
Cataracts are made of cells found naturally within the eye. When they clump together, they cause clouding and reduced vision.
What will happen if a cataract is left untreated?
Waiting for cataract surgery typically won’t hurt your eyes or make later surgery difficult. But the delay could keep you from everyday activities, like reading or driving.
Don't Let Cataracts Limit Your Life
With 135+ locations and over 2.5 million procedures performed, our board-certified cataract surgeons have the experience you can trust. Take the first step toward seeing clearly again.
Restore Clarity to your World Today.
References
- Cataracts. (January 2023). National Eye Institute.
- Cataract. (July 2022). StatPearls.
- Self-Reported Driving Difficulty in Patients with Bilateral Cataract. (December 2022). Journal of Optometry.
- Cataract in Adults. (December 2022). UpToDate.
- Types of Cataract. (January 2023). National Eye Institute.
- Maintaining Transparency: Study to Focus on Causes of Cataracts. (February 2022). National Eye Institute.
- Clinical Outcomes of Femtosecond Laser-Assisted Cataract Surgery Versus Conventional Phacoemulsification: A Retrospective Study in a Tertiary Eye Care Center in South India. (December 2022). Indian Journal of Ophthalmology.

John Davidson, M.D. is a board-certified ophthalmologist who has performed more than 50,000 eye procedures. He has been performing cataract surgery since 1988 and LASIK/PRK since 1999.
This content is for informational purposes only. It may have been reviewed by a licensed physician, but is not intended to serve as a substitute for professional medical advice. Always consult your healthcare provider with any health concerns. For more, read our Privacy Policy and Editorial Policy.

