Conjunctivitis: Causes and Real Treatments of Pink Eye
Home / Eye Conditions & Eye Diseases /
Last Updated:
The National Eye Institute (NEI) publishes that about 3 million Americans suffer from conjunctivitis, commonly called pink eye, each year, making it one of the most common eye conditions in the United States. Pink eye is so named because it causes irritation to the eye that can make it look red in color.
Table of Contents
Pink eye can be viral, bacterial, caused by irritants, or related to allergies. It is easily treatable and can impact both children and adults.
Conjunctivitis can be extremely contagious and passed to others through contact with eye fluids. Conjunctivitis may not always require a medical intervention, as it can sometimes be cleared up at home. Conjunctivitis does not typically impact vision, but if it does or if the pain and redness are significant, medical treatment and antibiotics can be helpful to clear it up.
Pink eye can be prevented and minimized through good hygiene practices. Conjunctivitis is usually not a serious condition. It can be cleared up quickly and without lasting damage.
What Is Conjunctivitis?
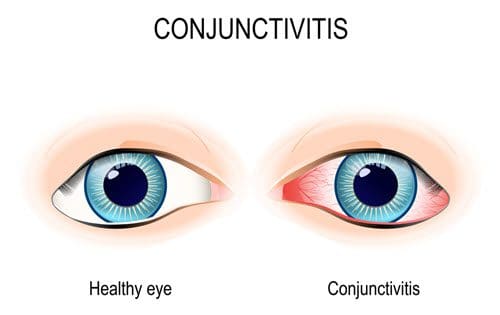
Conjunctivitis is an irritation or inflammation in the conjunctiva, which is the thin clear layer of tissue on the inside of the eyelid that covers the sclera of the eye, or the white part. When this gets inflamed, blood vessels are more visible. This makes the eye appear red or pink, giving conjunctivitis its common name of pink eye.
The American Optometric Association (AOA) reports that conjunctivitis is especially common in children. It is generally a minor eye infection, but if left untreated, it can be more serious and cause more significant issues. There are four main types of pink eye:
- Viral conjunctivitis
- Bacterial conjunctivitis
- Chemical conjunctivitis
- Allergic conjunctivitis
These forms of pink eye can impact both children and adults. Both the viral form and the bacterial form are easily spread from person to person.
Another form of pink eye that affects newborns, neonatal conjunctivitis, or ophthalmia neonatorum, typically appears within a day or up to two weeks after birth. It can be caused by a blocked tear duct in the eye, passed from the mother during birth (even if the mother is not showing symptoms), or caused by irritants getting into the eye soon after birth. Newborn conjunctivitis can also be caused by sexually transmitted diseases such as chlamydia and gonorrhea — chlamydial conjunctivitis and gonococcal conjunctivitis respectively.
The Centers for Disease Control and Prevention (CDC) warns that neonatal conjunctivitis can be very serious and requires immediate medical attention to prevent serious complications and vision issues. Neonatal conjunctivitis often needs to be treated with oral, topical, or even intravenous antibiotics.
Common Causes of Pink Eye
The cause of pink eye depends on the type of conjunctivitis.
- Viral conjunctivitis: Viral conjunctivitis is often related to the common cold and caused by a contagious virus, such as the flu, a cold, or a respiratory infection. NEI publishes that viral conjunctivitis is sometimes caused by the herpes virus or the adenovirus. Viral conjunctivitis typically begins in one eye first and then moves on to the other eye. It can be caused by exposure to coughing or sneezing from someone suffering from a respiratory infection. Viral pink eye can also be the result of a cold as the mucus membranes in the body are connected, including the conjunctiva the throat, lungs, nose, and tear ducts. Tears drain down through the nasal passageways. When you have a cold and then blow your nose, you can then move a respiratory infection up into your eyes, AOA explains.
- Bacterial conjunctivitis: Bacteria such as Streptococcus pneumonia, Haemophilus, or Staphylococcus aureus are common causes of bacterial pink eye. This typically comes from your own respiratory system or skin, and it can be spread through improper handwashing and then touching the eyes, insects, contact with other people, or poor hygiene. Using contaminated makeup or lotion, or sharing makeup or contacts with another person, can also spread bacterial conjunctivitis. Improperly cleaning your contacts or wearing them for too long may also lead to the onset of bacterial pink eye.
You deserve clear vision. We can help.
With 135+ locations and over 2.5 million procedures performed, our board-certified eye surgeons deliver results you can trust.
Your journey to better vision starts here.
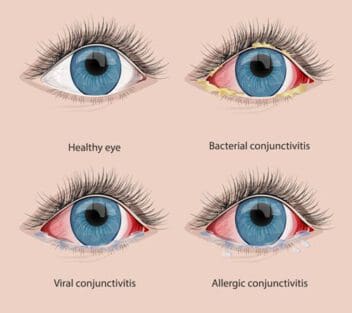
- Chemical conjunctivitis: Chemical conjunctivitis is caused by an irritant in the eye. Noxious chemicals, pool chlorine, and air pollution can all cause this form of pink eye. A chemical splash or exposure to a foreign object in the eye can cause chemical conjunctivitis, which is not contagious or spread by touch or from person to person.
- Allergic conjunctivitis: This form of pink eye is caused by a substance that can trigger an allergic reaction in the eyes, such as pollen. It most commonly impacts people who suffer from seasonal allergies. Mayo Clinic explains that when you are exposed to an allergen, your body produces immunoglobulin E (IgE), which is an antibody that interacts with mast cells in your airways and mucus linings of the eyes that then trigger the release of histamines, which are inflammatory substances. Allergic conjunctivitis can be caused by this allergic response in the body.
What Does Pink Eye Look Like? (Symptoms and Signs)
The most outwardly noticeable symptom of pink eye is the reddish or pink color of the eyes. Other symptoms include:
- Increased tearing.
- Discharge that can form a crust overnight and seem to “seal” the eye shut.
- Feeling like there is something “gritty” in the eye.
- Itchiness of the eye.
- Irritation or pain in the eye.
- Sensitivity to light.
- Swollen eyelids.
- Burning sensation in the eye.
- Contact lens discomfort.
Pink eye can impact one or both eyes, and it can range from mild to more significant. Pink eye usually resolves within one to two weeks, and it does not usually result in serious complications.
Treatments for Pink Eye: What to Do
The U.S. National Library of Medicine (NLM) publishes that conjunctivitis can often be treated at home and cleared up without medical treatment; however, bacterial conjunctivitis often needs medical care that will typically involve ointments or antibiotic eye drops. Viral conjunctivitis must run its course, and antibiotics or treatments will not speed up the process, but in some cases, antiviral medications may be helpful. If you wear contacts, you will most likely need to stop wearing them for a few days while the infection clears up.
Both viral and bacterial conjunctivitis are very contagious. They can be spread through contact with the eye fluid. If you have either of these forms of pink eye, you should avoid contact with other people for a few days while it clears up. Children should be kept home from school. A warm compress pressed gently on the eyes, made from a clean cloth soaked in warm water, can be soothing for conjunctivitis.
If conjunctivitis was caused by contact lens wear, you may need to switch to a different disinfection solution, type of lens, or even to a prescription that has you changing the lenses more often to prevent the infection from reoccurring. If you have been diagnosed with conjunctivitis, be careful not to touch your eyes, wash your hands often and thoroughly, throw away any makeup you have been putting on or near your eyes (especially mascara), change your washcloths and towels daily, keep your eyes clean by washing discharge regularly, try not to rub your eyes, and do not share cosmetics or eye care materials with others.
When to Seek Medical Attention for Conjunctivitis
If you have come in contact with a toxin or experienced a chemical burn to the eye, seek immediate medical attention. This can be a serious form of conjunctivitis that may create scarring to the eye or other vision problems. Bacterial conjunctivitis requires a prescription to clear up properly as well as medical care and a diagnosis for a prescription. If you suffer from significant eye pain or irritation, blurred vision, or intense sensitivity to light as a result of conjunctivitis, it is also time to see a doctor.
Once you start using self-care methods to take care of pink eye, it should start to improve within a day or two. If it does not, make an appointment with your doctor to get it checked out. If you have other medical conditions or issues that can compromise your immune system, such as cancer treatments or an HIV infection, then you should also make a point to see a health care provider when conjunctivitis is suspected.
You deserve clear vision. We can help.
With 135+ locations and over 2.5 million procedures performed, our board-certified eye surgeons deliver results you can trust.
Your journey to better vision starts here.
Methods for Preventing Conjunctivitis
Allergic conjunctivitis and chemical conjunctivitis are harder to prevent since they can be caused by airborne and foreign objects that may not be predictable or discernible ahead of time. Viral and bacterial pink eye are more common, however. There are some things you can do to prevent the spread of these contagious forms of conjunctivitis.

- Wash your hands with soap and water immediately upon contact with someone suffering from conjunctivitis.
- Keep your hands away from your eyes.
- Do not share contacts, eye glasses, eye makeup or cosmetics, facial lotions, or makeup brushes with others.
- Use your own towels, washcloths, pillowcases, and blankets, and wash them often.
- Follow the directions on your contact lenses. Change them as often as needed and disinfect them properly.
- Clean eyeglasses regularly and thoroughly.
Conjunctivitis in Newborns
Conjunctivitis can range from mild to serious but usually resolves within one to two weeks. Conjunctivitis in newborns can often result from dangerous bacteria. In these cases, it’s advisable to consult a doctor immediately to prevent permanent eye damage.
To prevent neonatal conjunctivitis, most hospitals will use an ointment on a newborn’s eyes. If a blocked tear duct is the cause of the condition, a gentle, warm massage between the eye and nasal area can help.
Frequently Asked Questions About Pink Eye
How can you prevent conjunctivitis?
Good hygiene, including proper handwashing, using clean tissues to wipe the face, and not sharing cosmetics, are some of the best ways to prevent and stop the transmission of conjunctivitis.
Can I still go to work or school if I have pink eye?
If you have conjunctivitis, but it does not present with a fever or other symptoms, you might be allowed to go to work with your doctor’s approval. However, pink eye is notorious for spreading in schools. It’s best to check with your doctor to determine when your child can return to school.
What happens if I don’t treat my pink eye?
Most uncomplicated cases of pinkeye can heal completely on their own, without long-term complications. But if conjunctivitis is a result of an underlying infection, the condition may recur over time. Untreated over a long time, it lead to vision loss. Medical professionals advise to seek treatment from a local health provider to secure any needed medication or treatment plan.
You deserve clear vision. We can help.
With 135+ locations and over 2.5 million procedures performed, our board-certified eye surgeons deliver results you can trust.
Your journey to better vision starts here.
References
- Facts About Pink Eye. (November 2015). National Eye Institute.
- Conjunctivitis. (2019). American Optometric Association.
- Conjunctivitis (Pink Eye) in Newborns. (January 2019). Centers for Disease Control and Prevention.
- Pink Eye (Conjunctivitis). (2019). Mayo Clinic.
- Pink Eye. (April 2018). U.S. National Library of Medicine.
- Conjunctivitis (Pink Eye). (January 4, 2019). Centers for Disease Control and Prevention.
- Facts about Pink Eye. (August 3, 2019) National Eye Institute.
- Pink Eye. (July 2021). Mayo Clinic.
This content is for informational purposes only. It may have been reviewed by a licensed physician, but is not intended to serve as a substitute for professional medical advice. Always consult your healthcare provider with any health concerns. For more, read our Privacy Policy and Editorial Policy.
