Retinal Detachment: Causes & How to Get Treatment
Home / Eye Conditions & Eye Diseases /
Last Updated:
All the pieces of your eye work together to deliver crisp vision, but there is a small layer of cells at the back of your eye that plays a critical role. The retina interprets light as it moves through the eye, and it translates that into electrical impulses your brain can understand.
Table of Contents
If the retina tears or buckles, it loses contact with nourishing blood flow. That is retinal detachment, and it’s a medical emergency.
In the past, retinal detachments almost always meant blindness. Surgeons tried to correct the problem, but they just didn’t have the tools or the technology to do so.
Now, surgeons have several different types of techniques they can lean on to fix a retinal detachment. In 9 out of 10 times, they can completely restore vision.
Those improvements are critical, as some retinal detachment risk factors — including myopia — are on the rise. You may not be able to prevent all the risks from hitting you, but there are some things you can do to keep your eyes safer.
What Is a Retinal Detachment?
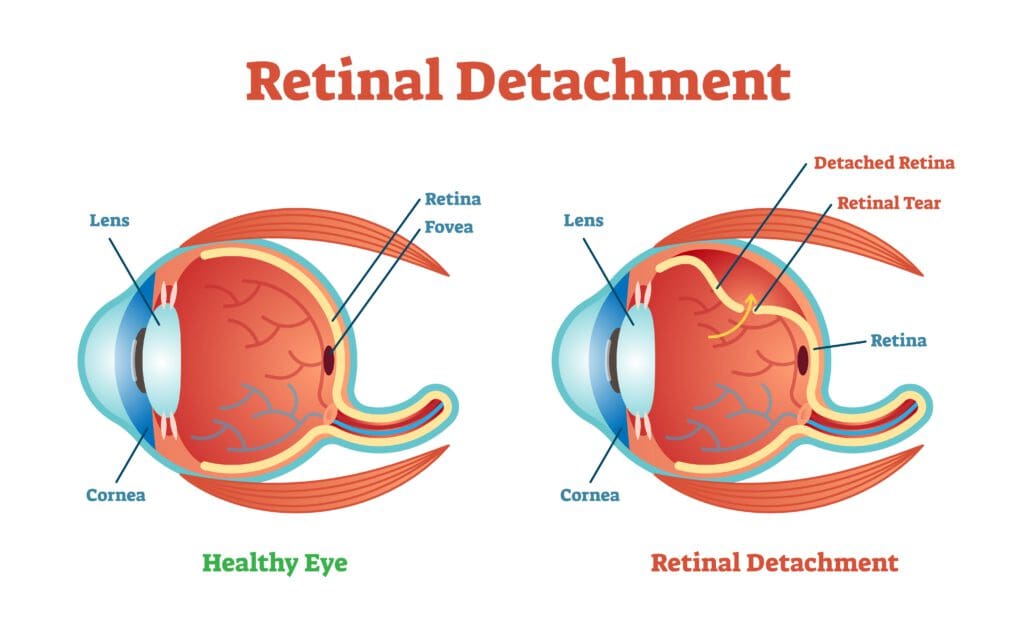
Think of your retina as the core of your eye. This thin piece of tissue translates light into electrical impulses, and it’s responsible for your ability to see. To stay functional, the retina needs constant contact with blood flow. If that is breached, it’s a retinal detachment.
The National Eye Institute says there are three different types.
You deserve clear vision. We can help.
With 135+ locations and over 2.5 million procedures performed, our board-certified eye surgeons deliver results you can trust.
Your journey to better vision starts here.
- Exudative: This form is often caused by disease or injury. The retina does not tear, but fluids leak between the retina, interrupting connection with blood flow.
- Rhegmatogenous: The retina tears or breaks, and that allows fluid to slide beneath. This is the most common type of detachment.
- Tractional: This is caused by retinal scars that contract. The movement pulls the retina away from nourishment.
All these types have different causes. Some involve pressure or a blow to the head, and others are sparked by disease or illness. But they all include some kind of separation or movement of retinal tissue away from nourishment.
Whenever the retina is pulled away, cells start to die. Lose enough of them, and you will also lose the ability to see.
What Does Detachment Feel Like?
Most medical emergencies come with severe symptoms. A heart attack, for example, is accompanied by shortness of breath and significant pain. Similarly, a stroke can cause extreme clumsiness and fainting.
A retinal detachment is different. The symptoms are subtle, and the one you might expect just does not exist.

Most retinal detachment symptoms involve your vision. You will notice:
- Floaters. Dark specks move through your field of vision. If you try to focus on them, they float away.
- Flashes. You will see bright spots of color across your visual field.
- Darkening. Something that looks like a shadow or a curtain will drop over your view. Typically, you will lose your peripheral vision first.
- Blurring. You will have trouble focusing on objects, even if you squint.
There is one symptom you might expect but will not feel: pain. According to Mayo Clinic, retinal detachments can be scary and cause panic. But they rarely cause physical pain in the eyes or the head.
Retinal Detachment in the Past
Retinal detachments are not new. People have struggled with this medical issue for decades. But years ago, people who had this issue rarely kept their vision. Medical technology wasn’t capable of providing a cure.
In a review published in the Scientific Journal of Medical and Vision Research, writers point out that 1 person in 1,000 with retinal detachment kept their vision in 1912. Doctors considered surgery a last-ditch effort to return vision, and it rarely worked.
Eye surgeons had to use large, handheld tools to help their patients in the 1910s and 1920s, and they didn’t have lasers and specialized visualization tools to help them scope out problems.
The retina and other eye tissues are small, delicate, and sensitive. Touching them in the wrong way means harming them. Often, early surgeries did just that.
You deserve clear vision. We can help.
With 135+ locations and over 2.5 million procedures performed, our board-certified eye surgeons deliver results you can trust.
Your journey to better vision starts here.
Retinal Detachment Now
Modern eye surgeries are incredibly sophisticated. Ophthalmologists have tools that their forbearers didn’t dream of. Now, doctors can repair almost all retinal detachment issues, and that is true even if the problem happens more than once.
The American Society of Retina Specialists says 9 in 10 cases of retinal detachment repairs are successful. Clearly, the new tools and new techniques can repair the damage a tear can do. And doctors have many different types of surgeries to choose from.
Surgeons can use:
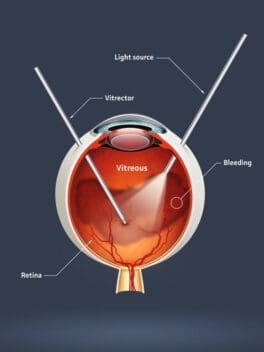
- Vitrectomy. Your surgeon removes the gel inside your eye and stitches up the tear. Then, oil or gas fills up the eye and holds the stitches in place until the eye heals.
- Scleral buckling. Your surgeon stitches bits of rubber or sponge onto your eye, and the tissue around it is frozen or heated to scar up the tissue.
- Freezing. Cryotherapy lets your surgeon freeze the tear in your retina and connect it to the back of your eye.
- Lasers. Tissue on either side of the tear is burned and scarred with a laser, so it shrinks and knits together.
These are sophisticated procedures, and you will need an ophthalmologist to do the work. This is not something a standard doctor or therapist can do. But they are often provided on an outpatient basis, so you can go home the same day. Depending on the type of surgery, recovery times vary.
Even if you need more than one surgery, you still have a great chance at clear vision. In a study from the Journal of Ophthalmology, researchers said 80 percent of people with multiple retinal detachment surgeries had successful procedures. The researchers noted that the number of operations didn’t relate to visual acuity.
This should be good news if you are worried about losing your sight due to retinal detachment. But it’s best to avoid the issue in the first place, and that is not always easy.
Causes & Risk Factors
Retinal detachment can happen to anyone, and there are some risk factors you can’t change. But there are a few things you can do to keep your eyes healthy.
The American Academy of Ophthalmology says retinal detachment risk factors include:
- The use of some glaucoma medications.
- Serious eye injuries.
- A family history of retinal detachment.
- Previous eye surgery.
- Nearsightedness.
There is one risk factor you can address in this list: eye injury. Always wear protective glasses when you are playing sports, tackling construction projects, and otherwise engaging in activities that could cause your eyes harm. And avoid roughhousing with people or pets.
Nearsightedness is a major risk factor for retinal detachment, and the National Eye Institute says the number of people with myopia has risen 25 percent since 1971. You can’t amend your risk of this condition, but if you have it, you can work with your doctor on exams. Annual checks help your doctor monitor the health of the back of your eye, and if a problem appears, early treatment could help.
If a retinal detachment happens, do not panic. Head to the doctor right away for swift surgery to correct the issue. And when you’ve healed, ask your doctor for advice on preventing a repeat episode. You might get tailored advice that prevents the problem before it starts again.
You deserve clear vision. We can help.
With 135+ locations and over 2.5 million procedures performed, our board-certified eye surgeons deliver results you can trust.
Your journey to better vision starts here.
References
- Facts About Retinal Detachment. (October 2009). National Eye Institute.
- Retinal Detachment. (March 2019). Mayo Clinic.
- Evolution of Retinal Detachment Surgery Down the Ages. (July 2017). Scientific Journal of Medical and Vision Research.
- Retinal Detachment. (2016). American Society of Retina Specialists.
- What You Need to Know About a Detached Retina. (January 2018). Medical News Today.
- Surgical and Visual Outcome for Recurrent Retinal Detachment Surgery. (2014). Journal of Ophthalmology.
- Retinal Detachment: Who Is at Risk for a Torn or Detached Retina? (May 2016). American Academy of Ophthalmology.
- Myopia: A Close Look at Efforts to Turn Back a Growing Problem. (October 2017). National Eye Institute.
This content is for informational purposes only. It may have been reviewed by a licensed physician, but is not intended to serve as a substitute for professional medical advice. Always consult your healthcare provider with any health concerns. For more, read our Privacy Policy and Editorial Policy.
